COVID-19 Vaccines: A Shield Against Long COVID?
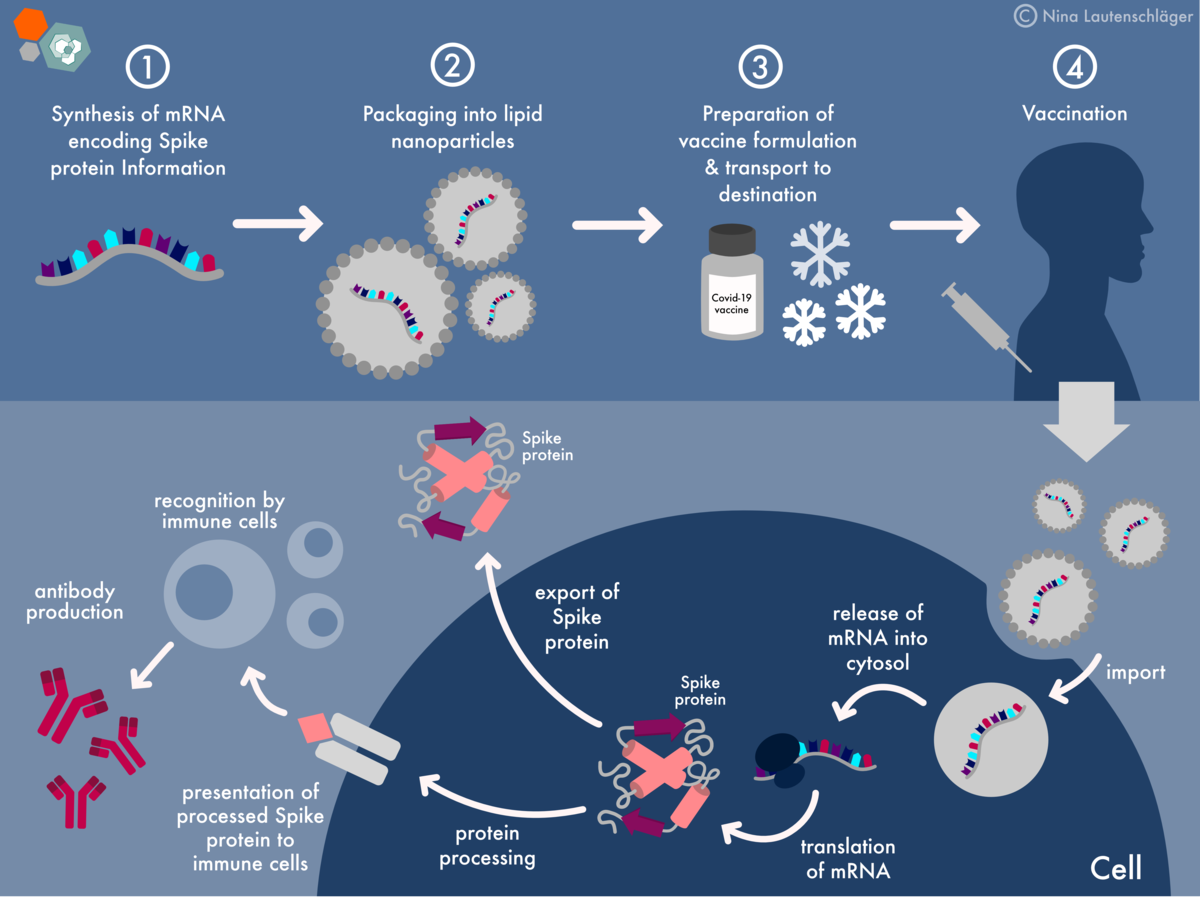
Table of Contents
Do COVID-19 Vaccines Reduce the Risk of Long COVID?
Evidence from Observational Studies
Numerous observational studies suggest a correlation between COVID-19 vaccination and a reduced risk of developing Long COVID. These studies, while not providing definitive proof of causation due to inherent limitations, offer compelling evidence.
- Study 1: A large-scale study published in the Lancet (cite specific study here) found that fully vaccinated individuals had a significantly lower risk of developing Long COVID compared to unvaccinated individuals. The study reported a [insert percentage]% reduction in risk.
- Study 2: Research published in the New England Journal of Medicine (cite specific study here) demonstrated a similar trend, showing that vaccination was associated with a reduced incidence of Long COVID across different age groups and demographics. [Insert specific findings here, e.g., a 30% reduction in risk of persistent fatigue].
- Study 3: [Cite another relevant study and its findings regarding Long COVID risk reduction and vaccine efficacy].
It's crucial to acknowledge limitations inherent in observational studies. Confounding factors, such as pre-existing health conditions or differences in social behaviors, can influence the results. Furthermore, different vaccine types (mRNA vaccines like Pfizer-BioNTech and Moderna, and viral vector vaccines like AstraZeneca and Johnson & Johnson) may exhibit varying degrees of effectiveness against Long COVID, a factor needing further research.
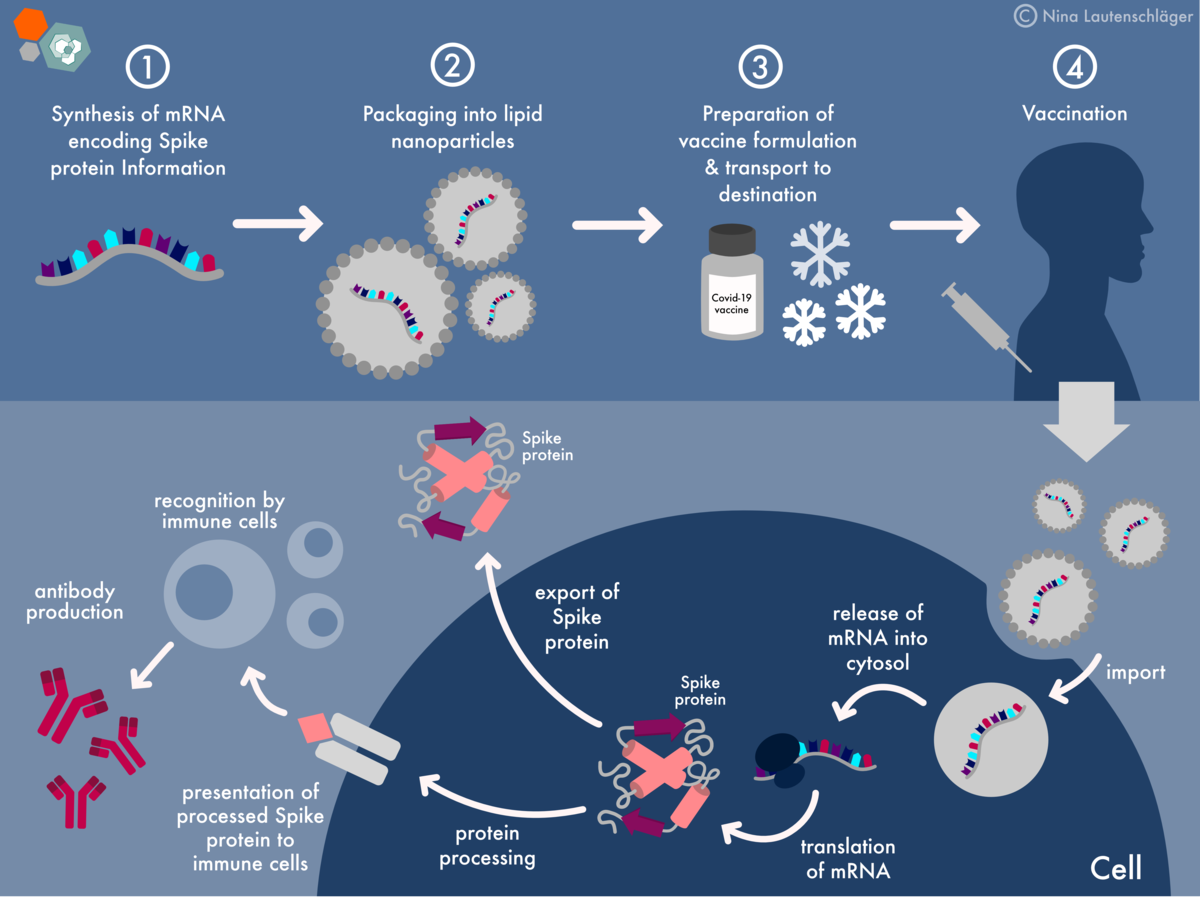
Mechanisms of Protection
Several mechanisms may explain how COVID-19 vaccination reduces Long COVID risk:
- Reduced Viral Load: Vaccines significantly reduce the viral load following infection, potentially limiting the duration and intensity of the inflammatory response that contributes to Long COVID.
- Improved Immune Response: Vaccination elicits a stronger and more rapid immune response, clearing the virus more efficiently and mitigating the likelihood of prolonged inflammation. This includes both a robust antibody response and a well-functioning T cell response, crucial for long-term immunological memory.
- Prevention of Severe Illness: By preventing severe COVID-19, vaccination indirectly reduces the risk of Long COVID, as severe infection is associated with a higher incidence of persistent symptoms.
Do Vaccines Reduce the Severity of Long COVID Symptoms?
Impact on Specific Symptoms
While reducing the risk of Long COVID is crucial, research is also exploring whether vaccination impacts the severity of symptoms in individuals who still develop the condition. Studies are ongoing, but some preliminary findings suggest potential benefits:
- Fatigue: Some studies indicate that vaccinated individuals experiencing Long COVID may experience less severe fatigue compared to their unvaccinated counterparts. [Cite studies if available, highlighting specific findings].
- Brain Fog: The impact of vaccination on brain fog remains an area of active investigation, with some studies showing potential, but inconclusive, positive effects. [Cite relevant studies and qualifications].
- Shortness of Breath: Similar to brain fog, the effect of vaccination on shortness of breath as a Long COVID symptom requires further research. [Mention ongoing studies and research needs].
It's important to note inconsistencies across studies, potentially due to differences in study designs, participant populations, and the specific Long COVID symptom being assessed. Further research is needed to fully elucidate the relationship between vaccination and symptom severity. Factors such as vaccine type, timing of vaccination (before or after infection), and individual factors like age and pre-existing conditions may also play a significant role.
Impact on Long-Term Health Outcomes
Research on the long-term effects of vaccination on Long COVID recovery is still in its early stages. However, preliminary data suggest that vaccination might positively influence long-term health outcomes:
- Faster Recovery: Some evidence hints that vaccinated individuals might experience faster recovery from Long COVID symptoms compared to unvaccinated individuals. [Cite studies if available].
- Reduced Risk of Complications: Vaccination may reduce the risk of developing serious long-term complications associated with Long COVID, such as cardiovascular issues or neurological problems. [Cite studies if available].
- Improved Quality of Life: By alleviating symptoms and potentially speeding up recovery, vaccination could ultimately lead to improved quality of life for individuals affected by Long COVID. More research is needed to confirm these potential benefits.
Addressing Concerns and Misinformation
Common Myths About COVID-19 Vaccines and Long COVID
Several myths and misconceptions surround the relationship between COVID-19 vaccines and Long COVID. It's essential to rely on credible sources like the CDC and WHO to dispel these inaccuracies.
- Myth 1: "COVID-19 vaccines cause Long COVID." Fact: There is no evidence supporting this claim. Vaccines prevent severe illness and reduce viral load, making Long COVID less likely.
- Myth 2: "Vaccines don't protect against Long COVID." Fact: While not a complete shield, accumulating evidence suggests vaccines significantly reduce the risk and potentially the severity of Long COVID.
- Myth 3: [Add another common myth and its factual counterpoint, citing CDC or WHO resources].
Importance of Continued Research
Understanding the complete relationship between COVID-19 vaccines and Long COVID requires continued research. Further studies are needed to:
- Investigate the long-term protective effects of different vaccine types.
- Determine the optimal vaccination strategies to minimize Long COVID risk.
- Identify potential biomarkers that predict Long COVID development and response to vaccination.
Conclusion:
Current evidence suggests that COVID-19 vaccination can significantly reduce the risk and potentially the severity of Long COVID. While research continues to refine our understanding of this complex relationship, the available data strongly supports the benefit of vaccination as a crucial tool in preventing and mitigating this debilitating condition. Observational studies have shown a lower incidence of Long COVID among vaccinated individuals, and the mechanisms of protection likely involve reduced viral load and improved immune response. Consult your healthcare provider to discuss the benefits of getting vaccinated and boosted against COVID-19 to protect yourself against Long COVID. Staying informed about the latest research on COVID-19 vaccines and Long COVID is crucial for making informed decisions about your health.
Featured Posts
-
 Why Middle Managers Are Essential For Company Success And Employee Well Being
May 29, 2025
Why Middle Managers Are Essential For Company Success And Employee Well Being
May 29, 2025 -
 Redaktorens Navn Hedret Som Arets Redaktor I Aftenposten
May 29, 2025
Redaktorens Navn Hedret Som Arets Redaktor I Aftenposten
May 29, 2025 -
 Ipa O Ilon Mask Apoxorei Apo Tin Kyvernisi Tramp Kritiki Sto Megalo Omorfo Nomosxedio
May 29, 2025
Ipa O Ilon Mask Apoxorei Apo Tin Kyvernisi Tramp Kritiki Sto Megalo Omorfo Nomosxedio
May 29, 2025 -
 Antisipasi Hujan Prakiraan Cuaca Jawa Barat 26 Maret 2024
May 29, 2025
Antisipasi Hujan Prakiraan Cuaca Jawa Barat 26 Maret 2024
May 29, 2025 -
 2025s Top Office Chairs Features Benefits And Buying Advice
May 29, 2025
2025s Top Office Chairs Features Benefits And Buying Advice
May 29, 2025
Latest Posts
-
 Illegal Hunting Operation Uncovered Near Manitoba Nunavut Border
May 30, 2025
Illegal Hunting Operation Uncovered Near Manitoba Nunavut Border
May 30, 2025 -
 Remote Lodge Break In Leads To Caribou Poaching Investigation Rcmp
May 30, 2025
Remote Lodge Break In Leads To Caribou Poaching Investigation Rcmp
May 30, 2025 -
 Rcmp Investigate Illegal Caribou Hunting Near Manitoba Nunavut Border
May 30, 2025
Rcmp Investigate Illegal Caribou Hunting Near Manitoba Nunavut Border
May 30, 2025 -
 Joy Smith Foundation Launches A Media Advisory
May 30, 2025
Joy Smith Foundation Launches A Media Advisory
May 30, 2025 -
 Photo Opportunity Joy Smith Foundation Announces Launch
May 30, 2025
Photo Opportunity Joy Smith Foundation Announces Launch
May 30, 2025
