Fungal Infections: A Growing Threat Of Antibiotic Resistance
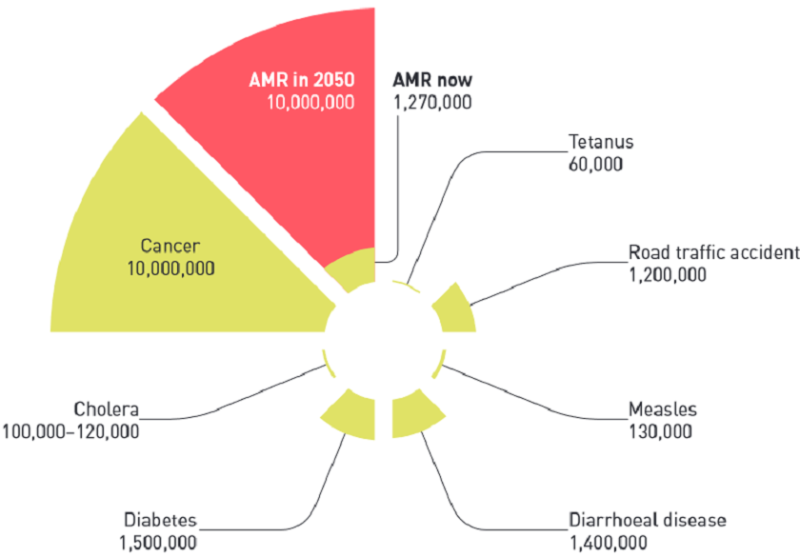
Table of Contents
The Rise of Antifungal Resistance
The effectiveness of antifungal drugs is waning due to the evolution of resistance mechanisms in fungi. This resistance poses a significant challenge to healthcare systems globally, prolonging illness, increasing mortality, and driving up healthcare costs.
Understanding Antifungal Resistance Mechanisms:
Fungi, like bacteria, develop resistance through various mechanisms. These include:
- Target site mutations: Alterations in the fungal cell's target site for the antifungal drug, rendering the drug ineffective. For example, mutations in the ERG11 gene, responsible for ergosterol synthesis, lead to azole resistance in Candida species.
- Efflux pumps: These cellular pumps actively expel antifungal drugs from the fungal cell, reducing the drug's intracellular concentration. This mechanism is common in many resistant fungal species, like Candida albicans.
- Reduced drug uptake: Changes in the fungal cell wall or membrane can reduce the uptake of antifungal drugs, minimizing their impact.
The genetic basis of these resistance mechanisms is complex and often involves multiple genes interacting. Understanding these mechanisms is crucial for developing new strategies to overcome resistance.
Factors Contributing to Antifungal Resistance:
Several factors contribute to the escalating problem of antifungal resistance:
- Overuse of antifungals: The widespread use of antifungals in both human medicine and agriculture selects for resistant strains. This is particularly concerning with azoles, which are commonly used in agriculture.
- Improper use of antifungals: Incorrect dosing, inappropriate treatment duration, and the use of broad-spectrum antifungals without proper diagnosis contribute to the development and spread of resistance.
- Lack of new drug development: The pipeline for new antifungal drugs is significantly limited compared to antibacterial drugs. This makes it harder to overcome existing resistance mechanisms.
- Increased use of antifungals in agriculture: The extensive use of azole antifungals in agriculture to protect crops contributes significantly to the selection and spread of resistant fungal strains.
The Impact of Fungal Infections on Human Health
Fungal infections range from superficial skin infections to life-threatening invasive diseases. Their impact on human health is substantial and growing, particularly in vulnerable populations.
High-Risk Populations:
Several groups are at significantly increased risk of developing serious fungal infections:
- Immunocompromised individuals: People with weakened immune systems, such as those with HIV/AIDS, undergoing chemotherapy, or organ transplant recipients, are highly susceptible to invasive fungal infections.
- Patients with chronic illnesses: Individuals with diabetes, chronic lung diseases, or other chronic conditions are more vulnerable to fungal infections.
- Neonates and infants: Newborns and infants have immature immune systems, making them prone to fungal infections.
Mortality rates for invasive fungal infections are high, highlighting the urgent need for effective prevention and treatment strategies.
Severity and Mortality of Fungal Infections:
Certain fungal infections are associated with high morbidity and mortality. Examples include:
- Invasive aspergillosis: A severe infection caused by Aspergillus fungi, particularly threatening to immunocompromised individuals. Mortality rates can exceed 50%.
- Candidiasis: Infections caused by Candida species, ranging from superficial thrush to life-threatening bloodstream infections (candidemia).
- Cryptococcal meningitis: A severe fungal meningitis, primarily affecting individuals with HIV/AIDS.
These infections often require prolonged and intensive treatment, leading to substantial healthcare burdens.
Current and Future Strategies to Combat Antifungal Resistance
Combating the growing threat of antifungal resistance requires a multi-pronged approach encompassing research, improved stewardship, and public health initiatives.
Developing New Antifungal Drugs:
The discovery and development of novel antifungal drugs with new mechanisms of action is crucial. This includes:
- Targeting unique fungal pathways: Identifying and targeting fungal-specific metabolic pathways that are not present in humans.
- Repurposing existing drugs: Exploring the potential of existing drugs for use against fungal infections.
- Developing combination therapies: Combining different antifungal drugs to overcome resistance mechanisms.
Significant challenges remain in antifungal drug development, including the complex biology of fungi and the inherent difficulties in developing drugs that specifically target fungal cells without harming human cells.
Improving Antifungal Stewardship:
Responsible use of antifungals is critical to preventing the emergence and spread of resistance. Key strategies include:
- Accurate diagnosis: Using appropriate diagnostic techniques to identify the fungal pathogen and its susceptibility profile before initiating treatment.
- Targeted therapy: Prescribing the most appropriate antifungal drug and dose based on the identified pathogen and its susceptibility.
- Infection control: Implementing robust infection control measures in healthcare settings to prevent the spread of fungal infections.
- Education and training: Educating healthcare professionals about appropriate antifungal use and infection prevention.
Public Health Initiatives:
Global collaboration and public health interventions are essential to effectively addressing the threat of antifungal resistance:
- Surveillance programs: Establishing and strengthening surveillance systems to monitor the prevalence of antifungal resistance.
- Education campaigns: Raising public awareness about fungal infections and the importance of preventing their spread.
- International collaboration: Fostering collaborations between researchers, healthcare professionals, and public health agencies to share knowledge and resources.
Conclusion:
The rise of antifungal resistance represents a significant threat to global health. The increasing prevalence of drug-resistant fungal infections, coupled with the limited pipeline of new antifungal drugs, underscores the urgency of addressing this critical challenge. We must prioritize the development of new antifungal agents, enhance antifungal stewardship practices, and strengthen public health interventions to combat fungal infections and prevent antifungal resistance. By understanding fungal infection threats and supporting research initiatives, we can work collectively to mitigate this growing public health crisis and promote responsible antifungal use, preventing further spread of resistance and improving patient outcomes. The time to act is now, to prevent a future where even common fungal infections become life-threatening.
Featured Posts
-
 Top Ps 5 Pro Enhanced Games A Must Play List
May 08, 2025
Top Ps 5 Pro Enhanced Games A Must Play List
May 08, 2025 -
 Barcelona Vs Inter Milan Champions League Semifinal Result And Analysis
May 08, 2025
Barcelona Vs Inter Milan Champions League Semifinal Result And Analysis
May 08, 2025 -
 Where Does Rogue Truly Belong Re Examining Her Marvel Allegiance
May 08, 2025
Where Does Rogue Truly Belong Re Examining Her Marvel Allegiance
May 08, 2025 -
 The Potential Of The Ps 5 Pro Hardware And Software Upgrades
May 08, 2025
The Potential Of The Ps 5 Pro Hardware And Software Upgrades
May 08, 2025 -
 Kratkaya Istoriya Matchey Arsenal Ps Zh V Evrokubkakh
May 08, 2025
Kratkaya Istoriya Matchey Arsenal Ps Zh V Evrokubkakh
May 08, 2025
Latest Posts
-
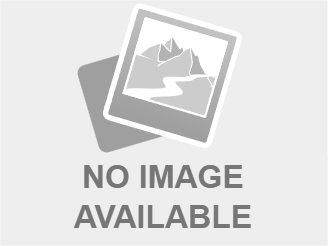
 Predicted Counting Crows Setlist For 2025 Concerts
May 08, 2025
Predicted Counting Crows Setlist For 2025 Concerts
May 08, 2025 -
 Counting Crows Potential 2025 Tour Setlist A Fans Speculation
May 08, 2025
Counting Crows Potential 2025 Tour Setlist A Fans Speculation
May 08, 2025 -
 Counting Crows 2025 Setlist Predictions What Songs Will They Play
May 08, 2025
Counting Crows 2025 Setlist Predictions What Songs Will They Play
May 08, 2025 -
 Analyzing Counting Crows Slip Into The Shadows From The Aurora Album A Track By Track Look
May 08, 2025
Analyzing Counting Crows Slip Into The Shadows From The Aurora Album A Track By Track Look
May 08, 2025 -
 Nba Playoffs Triple Doubles Quiz How Many Can You Name
May 08, 2025
Nba Playoffs Triple Doubles Quiz How Many Can You Name
May 08, 2025
