Measles Persistence: A Public Health Challenge And Its Solutions

Table of Contents
Factors Contributing to Measles Persistence
The continued presence of measles globally, despite readily available vaccines, is a complex issue stemming from interconnected factors. Understanding these contributing elements is crucial for developing effective interventions.
Vaccine Hesitancy and Misinformation
The rise of anti-vaccine movements and the proliferation of misinformation pose significant obstacles to measles eradication. Social media platforms, in particular, have become breeding grounds for false claims about vaccine safety and efficacy, fueling vaccine hesitancy and impacting vaccination rates.
- Impact of celebrity endorsements of anti-vaccine views: High-profile individuals promoting unfounded concerns about vaccines significantly influence public perception and erode trust in established medical expertise.
- Role of online echo chambers: Algorithmic filtering on social media reinforces pre-existing beliefs, creating echo chambers where misinformation spreads unchecked and counterarguments are rarely encountered.
- Effectiveness of counter-misinformation campaigns: While efforts to debunk false claims exist, their effectiveness varies, highlighting the need for more sophisticated and targeted communication strategies. These campaigns must address the underlying reasons for vaccine hesitancy and build trust through credible sources.
Gaps in Vaccination Coverage
Incomplete vaccination coverage, particularly in underserved populations, creates pockets of vulnerability where measles can easily spread. Geographic isolation, poverty, and lack of access to healthcare services disproportionately affect vaccination rates in certain communities.
- Importance of targeted vaccination campaigns: Reaching remote or marginalized communities requires tailored strategies, including mobile vaccination units and community-based outreach programs.
- Role of healthcare infrastructure: Robust healthcare infrastructure is vital for ensuring equitable access to vaccines and timely vaccination services. Strengthening healthcare systems in underserved areas is paramount.
- Addressing socioeconomic barriers to vaccination: Socioeconomic factors such as poverty, lack of education, and limited access to transportation can significantly impede vaccine uptake. Addressing these barriers requires multi-sectoral collaboration and targeted interventions.
Challenges in Surveillance and Outbreak Response
Effective measles control depends on robust surveillance systems and rapid response mechanisms. However, challenges in tracking and responding to outbreaks, particularly in resource-limited settings, hinder control efforts.
- Limitations of existing surveillance systems: Many countries lack the capacity for comprehensive and timely measles surveillance, leading to delayed detection and response to outbreaks.
- Importance of early detection and isolation: Prompt identification and isolation of cases are critical for preventing further spread. This requires well-trained healthcare workers and effective communication channels.
- Need for improved data sharing and collaboration: Real-time data sharing and collaboration among healthcare providers, public health officials, and international organizations are essential for effective outbreak response.
Strategies for Combating Measles Persistence
Eliminating measles requires a multi-pronged approach that addresses the underlying causes of its persistence and strengthens existing control measures.
Strengthening Vaccination Programs
Improving vaccine access and uptake is fundamental to measles control. This involves comprehensive strategies that go beyond simply providing vaccines.
- Integration of measles vaccination into existing healthcare programs: Routine immunization schedules should prioritize measles vaccination, ensuring that all children receive the necessary doses.
- Use of mobile vaccination units: Mobile vaccination clinics can reach remote and underserved communities, overcoming geographical barriers to vaccination.
- Incentivizing vaccination: Providing incentives, such as conditional cash transfers or other benefits, can encourage vaccine uptake, particularly in communities with low vaccination rates.
Addressing Vaccine Hesitancy
Building trust and addressing vaccine hesitancy through education and community dialogue is crucial. This requires engaging with communities and providing accurate, accessible information.
- Development of effective communication strategies: Tailored communication strategies, using trusted messengers and appropriate channels, can effectively address specific concerns and misconceptions about vaccines.
- Training healthcare providers on vaccine safety and efficacy: Healthcare providers play a crucial role in building trust and providing accurate information about vaccines.
- Utilizing trusted community leaders: Community leaders and influencers can effectively convey messages about vaccine safety and importance, particularly in culturally diverse settings.
Improving Surveillance and Outbreak Response
Investing in robust surveillance systems and rapid response teams is vital for preventing and controlling measles outbreaks. This includes strengthening laboratory capacity and improving data sharing.
- Development of early warning systems: Early warning systems can detect outbreaks early, enabling prompt intervention and preventing widespread transmission.
- Strengthening laboratory capacity: Well-equipped laboratories are essential for accurate and timely diagnosis of measles cases.
- Improving case investigation and contact tracing: Effective case investigation and contact tracing help identify and monitor individuals exposed to the virus, preventing further spread.
Conclusion
Measles persistence is a complex public health challenge driven by vaccine hesitancy, gaps in vaccination coverage, and limitations in surveillance and outbreak response. Combating measles persistence requires a multi-faceted approach. By addressing vaccine hesitancy through evidence-based communication, strengthening immunization programs through increased access and community engagement, and improving surveillance and outbreak response through enhanced data systems and rapid response teams, we can work towards a future free from this preventable disease. Let's all contribute to ending measles persistence through responsible vaccination practices and community engagement. Get vaccinated, support vaccination efforts in your communities, and advocate for policies that promote vaccine access and uptake.

Featured Posts
-
 Alcaraz Vs Musetti Rolex Monte Carlo Masters 2025 Final Preview
May 30, 2025
Alcaraz Vs Musetti Rolex Monte Carlo Masters 2025 Final Preview
May 30, 2025 -
 Integrale Europe 1 Soir 19 03 2025 Podcast Et Replay
May 30, 2025
Integrale Europe 1 Soir 19 03 2025 Podcast Et Replay
May 30, 2025 -
 Home And Garden Show Realtors Return To State Fair Park
May 30, 2025
Home And Garden Show Realtors Return To State Fair Park
May 30, 2025 -
 Dana White Needs To Pay Up Ufc Veteran On Jon Joness 29 Million Demand
May 30, 2025
Dana White Needs To Pay Up Ufc Veteran On Jon Joness 29 Million Demand
May 30, 2025 -
 Sosyal Medya Cilgina Doendue Pinar Deniz Ve Kaan Yildirim In Bebek Fotografi
May 30, 2025
Sosyal Medya Cilgina Doendue Pinar Deniz Ve Kaan Yildirim In Bebek Fotografi
May 30, 2025
Latest Posts
-
 Munichs Bmw Open 2025 Zverev Battles Griekspoor In Quarter Finals
May 31, 2025
Munichs Bmw Open 2025 Zverev Battles Griekspoor In Quarter Finals
May 31, 2025 -
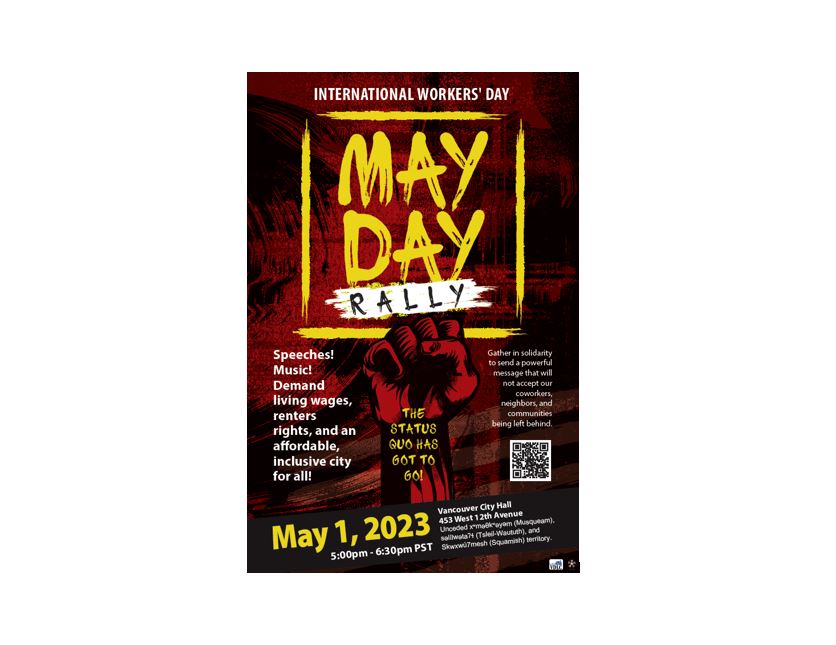 May Day Rally In Kingston Images Show Strength And Solidarity Daily Freeman
May 31, 2025
May Day Rally In Kingston Images Show Strength And Solidarity Daily Freeman
May 31, 2025 -
 Bmw Open 2025 Zverev Griekspoor Quarter Final Showdown In Munich
May 31, 2025
Bmw Open 2025 Zverev Griekspoor Quarter Final Showdown In Munich
May 31, 2025 -
 Indian Wells Surprise Zverevs First Match Exit And His Honest Assessment
May 31, 2025
Indian Wells Surprise Zverevs First Match Exit And His Honest Assessment
May 31, 2025 -
 Trump Administration Loses Key Advisor Elon Musks Resignation Explained
May 31, 2025
Trump Administration Loses Key Advisor Elon Musks Resignation Explained
May 31, 2025
