Mental Health Claim Rates: High Costs And Stigma Limit Access

Table of Contents
The High Cost of Mental Healthcare: A Major Barrier to Access
The prohibitive cost of mental healthcare acts as a significant barrier preventing many from seeking necessary treatment. This financial burden impacts individuals across all socioeconomic levels, but disproportionately affects those with lower incomes.
Insurance Coverage Gaps and Limitations
Inadequate insurance coverage for mental health services is a widespread issue. Many insurance plans have significant limitations that restrict access:
- High deductibles and copays: The initial out-of-pocket expenses required before insurance coverage begins are often substantial, creating an immediate financial hurdle for many.
- Limited number of covered sessions: Many plans restrict the number of therapy sessions covered annually, forcing individuals to pay out-of-pocket for additional sessions, even if clinically necessary.
- Narrow networks of providers: Insurance networks often limit access to specific mental health professionals, making it difficult to find a provider who meets an individual's needs and preferences.
- Exclusion of specific treatments: Some plans may not cover certain types of therapy or medication, further restricting treatment options.
For example, a policy might cover only 10 therapy sessions per year with a $100 copay per session, and a high deductible of $5,000. This means an individual would need to pay $1,000 before their insurance even begins to cover a portion of the cost of therapy.
The Price of Treatment
Even with insurance, the cost of mental healthcare remains high.
- Therapy costs: The hourly rate for therapy varies widely depending on the therapist's experience and location, but can easily range from $100 to $300 per session.
- Medication costs: Prescription medications for mental health conditions can be expensive, even with insurance coverage. Generic versions may be more affordable but may not always be suitable.
- Hospitalization costs: Inpatient mental health treatment is incredibly expensive, often requiring substantial out-of-pocket payments even with insurance.
These costs frequently surpass those associated with comparable physical healthcare treatments, creating a stark disparity in accessibility.
The Persistent Stigma Surrounding Mental Illness: A Silent Barrier
Beyond the financial hurdles, the persistent stigma surrounding mental illness acts as a powerful, silent barrier to seeking help. This stigma manifests in various ways, deterring individuals from accessing necessary care.
Societal Attitudes and Discrimination
Negative societal attitudes towards mental illness are deeply ingrained, often leading to:
- Misconceptions and misinformation: Widespread misconceptions about mental illness fuel prejudice and fear.
- Discrimination in employment and housing: Individuals with mental health conditions often face discrimination in the workplace and housing markets.
- Social isolation and exclusion: The stigma can lead to social isolation and prevent individuals from seeking support networks.
Fear of Judgment and Social Isolation
The fear of judgment and potential social repercussions significantly inhibits help-seeking.
- Fear of losing relationships: Individuals worry that disclosing their mental health struggles will strain relationships with family, friends, and colleagues.
- Concerns about career repercussions: There's a fear of negative impact on career prospects if mental health issues are disclosed.
- Shame and self-blame: Many individuals internalize societal stigma, leading to feelings of shame and self-blame.
The Impact of Low Mental Health Claim Rates
The consistently low mental health claim rates have far-reaching consequences:
Increased Burden on the Healthcare System
Untreated mental health conditions can lead to:
- Increased healthcare costs in the long run: Delayed or inadequate treatment often results in more severe illnesses, requiring more intensive and costly interventions.
- Reduced productivity and economic impact: Mental illness significantly impacts productivity, leading to lost workdays and decreased economic output.
- Increased strain on emergency services: Individuals with untreated mental health conditions may end up in emergency rooms, placing a strain on already overwhelmed healthcare systems.
Negative Impact on Individual Well-being
Limited access to mental healthcare has devastating personal consequences:
- Reduced quality of life: Untreated mental health conditions significantly impact relationships, work performance, and overall well-being.
- Increased risk of suicide and self-harm: Lack of access to timely and adequate care significantly increases the risk of suicide and self-harm.
- Chronic health problems: Untreated mental health conditions can lead to co-occurring physical health problems, further complicating healthcare needs.
Potential Solutions to Increase Mental Health Claim Rates
Addressing the crisis of low mental health claim rates requires a multi-faceted approach focusing on both improving access and reducing stigma:
Improving Mental Healthcare Access
- Policy changes to improve insurance coverage: Legislation mandating broader mental healthcare coverage, parity with physical healthcare, and eliminating unnecessary restrictions is crucial.
- Increased funding for mental health services: Investing in mental health services expands capacity, reduces waiting times, and increases accessibility for all.
- Promoting telehealth and remote mental health services: Expanding access through telemedicine platforms extends mental healthcare reach to underserved communities and individuals facing barriers to in-person care.
Reducing Stigma and Promoting Mental Health Awareness
- Public awareness campaigns: Initiatives that address misconceptions and promote understanding can destigmatize mental illness and encourage help-seeking.
- Education and open conversations: Integrating mental health education into schools and workplaces normalizes discussion and fosters empathy.
- Community support and resources: Developing community-based support groups and resources offers accessible and localized support systems.
Conclusion: Addressing the Crisis: Improving Access to Mental Healthcare
High costs and persistent stigma represent significant barriers to accessing mental healthcare, resulting in low mental health claim rates and substantial negative consequences for individuals and society. Addressing this crisis requires a comprehensive strategy: policy changes to improve insurance coverage, increased funding for mental health services, proactive efforts to reduce stigma through education and awareness campaigns, and increased access to a broader range of mental health services, including telehealth. We urge you to learn more about mental health resources in your community, advocate for policies that improve access to affordable mental healthcare, and engage in conversations to reduce the stigma surrounding mental illness. Together, we can help improve mental health claim rates and create a more supportive and equitable system of care for all. [Link to NAMI (National Alliance on Mental Illness)] [Link to MentalHealth.gov]

Featured Posts
-
 Harry Potters Crabbe Actors Stunning Transformation
May 03, 2025
Harry Potters Crabbe Actors Stunning Transformation
May 03, 2025 -
 Is Eyelash Shaving Becoming More Common Among Men
May 03, 2025
Is Eyelash Shaving Becoming More Common Among Men
May 03, 2025 -
 Russell T Davies On Doctor Whos Future A Potential Pause
May 03, 2025
Russell T Davies On Doctor Whos Future A Potential Pause
May 03, 2025 -
 Alan Roden A Study Of His Articles And Essays Published In The Spectator
May 03, 2025
Alan Roden A Study Of His Articles And Essays Published In The Spectator
May 03, 2025 -
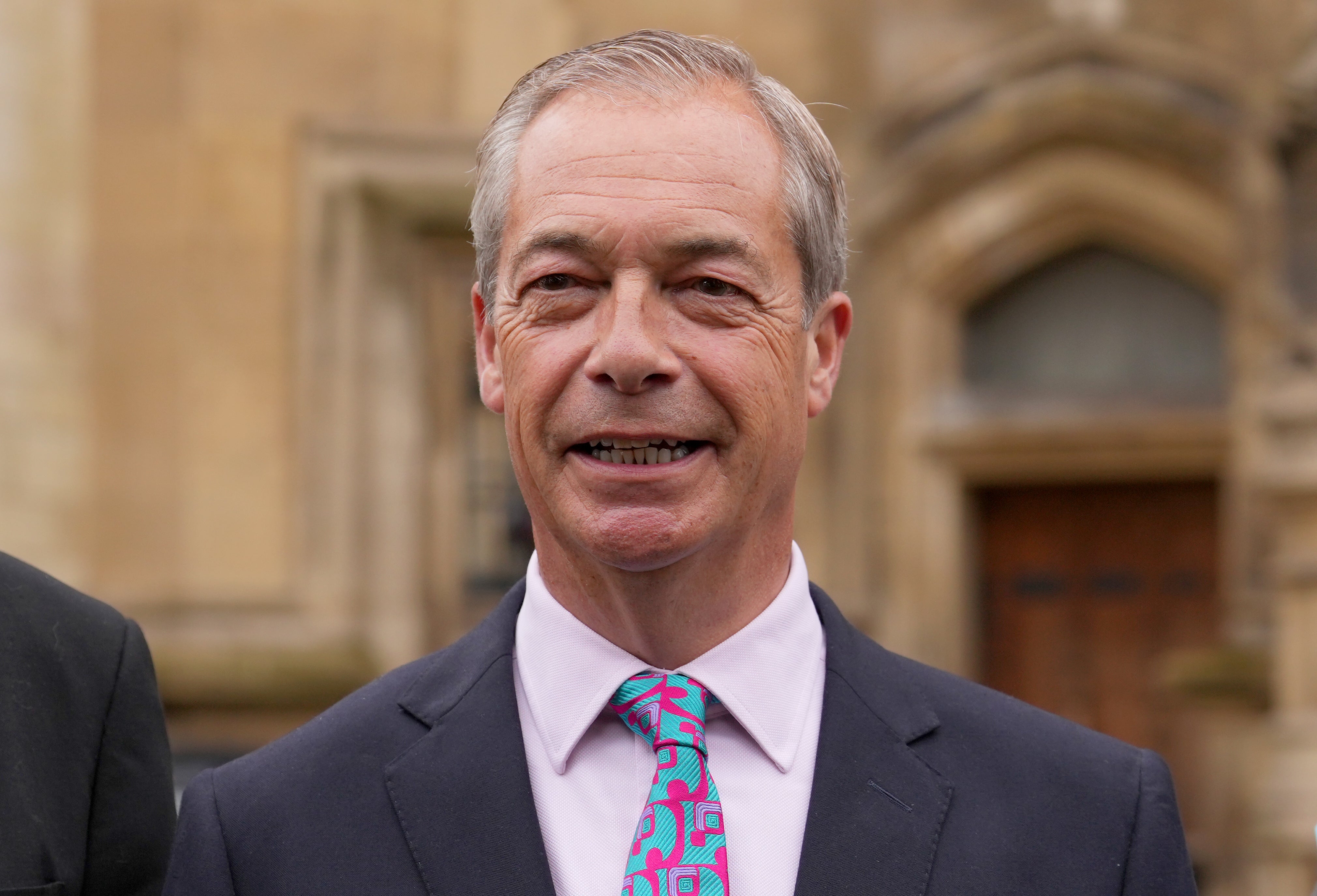
 Shrewsbury Visit Nigel Farage Criticizes Conservatives Enjoys Local Pub
May 03, 2025
Shrewsbury Visit Nigel Farage Criticizes Conservatives Enjoys Local Pub
May 03, 2025
Latest Posts
-
 A Place In The Sun Your Checklist For Buying Abroad
May 03, 2025
A Place In The Sun Your Checklist For Buying Abroad
May 03, 2025 -
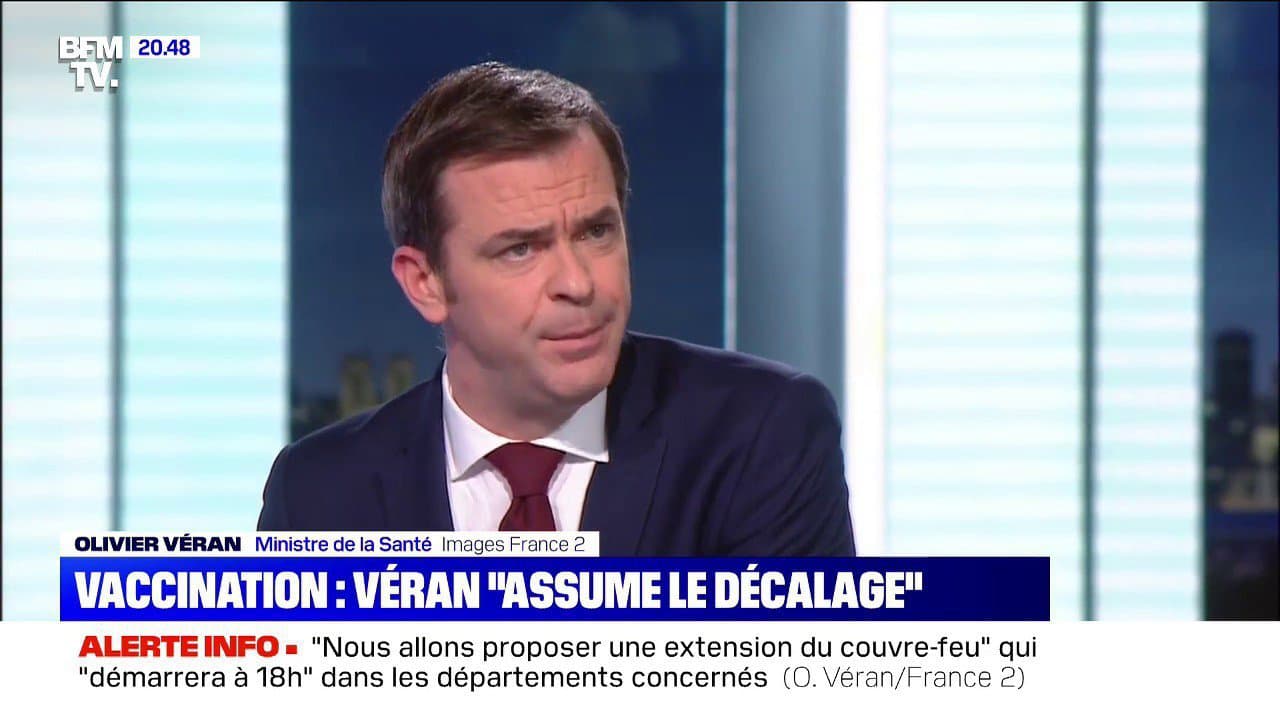 Rome Soupcons De Complot Macronien Pour Le Conclave Papal
May 03, 2025
Rome Soupcons De Complot Macronien Pour Le Conclave Papal
May 03, 2025 -
 Finding Your Place In The Sun A Guide To Overseas Property
May 03, 2025
Finding Your Place In The Sun A Guide To Overseas Property
May 03, 2025 -
 Reform Uk Five Reasons For Its Current Political Vulnerability
May 03, 2025
Reform Uk Five Reasons For Its Current Political Vulnerability
May 03, 2025 -
 L Intimite D Emmanuel Et Brigitte Macron Revelations Apres Des Annees De Vie Commune
May 03, 2025
L Intimite D Emmanuel Et Brigitte Macron Revelations Apres Des Annees De Vie Commune
May 03, 2025
