Mental Health Claims: Low Rates, High Costs, And The Stigma Barrier

Table of Contents
The staggering reality is that while mental health conditions affect millions, the number of mental health claims remains surprisingly low. This paradox – high costs associated with untreated mental illness despite low utilization rates of mental health services – points to a critical underlying issue: the pervasive stigma surrounding mental health. This article will explore the reasons behind the low rates of mental health claims, the significant financial implications of this under-treatment, and the crucial role of stigma in perpetuating this troubling problem.
H2: The Low Rate of Mental Health Claims: A Deep Dive
H3: Underdiagnosis and Lack of Access:
Many individuals struggle to access the mental healthcare they need. This "treatment gap" is a significant contributor to the low rate of mental health claims.
- Difficulty accessing affordable mental healthcare: The cost of therapy, medication, and other mental health services can be prohibitive, particularly for those without adequate insurance coverage.
- Long wait times for appointments: Finding a therapist or psychiatrist who accepts your insurance and has available appointments can take weeks or even months, deterring many from seeking help.
- Geographical limitations: Access to qualified mental health professionals is unevenly distributed, particularly in rural and underserved areas.
- Lack of awareness of available resources: Many individuals are unaware of the types of mental health services available, where to find them, or how to access them.
The challenges are substantial. Finding a therapist who accepts your specific insurance plan can feel like navigating a maze. Complex insurance procedures, pre-authorizations, and confusing billing practices often add to the burden, discouraging individuals from seeking necessary care. This lack of access directly impacts the number of mental health claims filed.
H3: Financial Barriers and Insurance Coverage:
High costs are a major impediment to accessing mental healthcare. Inadequate insurance coverage further exacerbates the problem.
- High out-of-pocket costs: Even with insurance, high deductibles, co-pays, and other out-of-pocket expenses can make mental healthcare unaffordable for many.
- Inadequate insurance coverage for mental health services: Many insurance plans provide limited coverage for mental health services compared to physical health services, creating a significant financial barrier.
- Limited network of providers accepted by insurance plans: Individuals may be restricted to a limited network of providers within their insurance plan, potentially limiting their choice of therapist or psychiatrist.
The impact of these financial barriers is profound. Many individuals delay or forgo treatment altogether due to the high cost, leading to the low number of mental health claims. Solutions like improved insurance parity legislation and increased funding for affordable mental health services are crucial to address this issue.
H3: The Role of Systemic Issues:
Systemic issues within the healthcare system contribute to the underutilization of mental health services.
- Shortage of mental health professionals: There is a significant shortage of psychiatrists, psychologists, and other mental health professionals, particularly in underserved areas.
- Insufficient funding for mental health services: Inadequate funding for mental health programs and services limits the availability and accessibility of care.
- Complex and confusing healthcare systems: Navigating the healthcare system, especially concerning mental health, can be overwhelming and confusing for many, leading to delays or avoidance of treatment.
These systemic issues necessitate significant policy changes and increased investment in mental health infrastructure. Expanding access to telehealth services, improving provider training and recruitment, and simplifying healthcare systems can all play a vital role in increasing mental health claim rates.
H2: The High Cost of Mental Health Conditions Left Untreated
H3: Increased Healthcare Utilization for Related Issues:
Untreated mental health conditions often lead to a cascade of negative consequences, significantly increasing healthcare costs.
- Untreated mental health conditions can lead to physical health problems: Mental health issues are frequently linked to physical health problems like heart disease, diabetes, and chronic pain, requiring additional medical care.
- Substance abuse: Individuals with untreated mental health conditions are at increased risk of substance abuse, adding further complications and healthcare costs.
- Increased emergency room visits: Mental health crises can lead to increased emergency room visits, resulting in high costs and potentially inefficient use of emergency services.
The cumulative effect of these related issues dramatically increases healthcare utilization and long-term healthcare costs. Early intervention and access to comprehensive mental health services are crucial to prevent these cascading effects and reduce the overall financial burden.
H3: Lost Productivity and Economic Impact:
The economic consequences of untreated mental illness are substantial, extending beyond individual healthcare costs.
- Mental health issues can lead to absenteeism: Untreated mental health conditions often lead to missed workdays and reduced productivity.
- Reduced productivity: Even when at work, individuals with untreated mental health conditions may experience reduced productivity and performance.
- Unemployment: Severe mental health conditions can lead to unemployment, resulting in loss of income and increased reliance on social support systems.
The collective impact on the economy includes lost wages, decreased workforce participation, and increased societal burden. Investing in mental healthcare is not just a matter of compassion, but also a matter of sound economic policy – yielding a significant return on investment (ROI) through increased productivity and reduced healthcare costs.
H2: Breaking Down the Stigma Barrier
H3: Understanding and Addressing the Stigma:
The stigma surrounding mental illness is a major barrier to help-seeking behavior.
- Misconceptions: Many misconceptions and misunderstandings surround mental illness, leading to prejudice and discrimination.
- Discrimination: Individuals with mental health conditions often face discrimination in employment, housing, and social settings.
- Fear of judgment: The fear of judgment and social isolation prevents many from seeking help.
Addressing this stigma requires multifaceted strategies, including public awareness campaigns, education initiatives, and promoting open conversations about mental health. Increased mental health literacy is crucial in challenging misconceptions and fostering a more supportive and understanding society.
H3: Promoting Open Conversations and Support:
Open communication and access to support are essential for breaking down the stigma.
- Encourage open conversations about mental health: Normalizing conversations about mental health helps reduce the stigma and encourages help-seeking behavior.
- Promote seeking professional help: Emphasize that seeking professional help is a sign of strength, not weakness.
- Highlight the availability of support systems: Make individuals aware of the range of support systems available, including helplines, online resources, and support groups.
Practical steps include reaching out to friends, family, or mental health professionals. Utilizing available online resources and support groups can provide valuable connection and aid in navigating challenges. Advocating for improved access to mental health services can help create a more supportive environment for all.
3. Conclusion:
The low rates of mental health claims, coupled with the high costs associated with untreated mental illness, highlight a critical public health challenge. Stigma plays a significant role in perpetuating this cycle, hindering access to timely and effective mental health treatment. Addressing this requires a multi-pronged approach: increased funding for mental health services, improved insurance coverage, addressing systemic issues within the healthcare system, and sustained efforts to reduce the stigma surrounding mental illness. We must all play our part – seeking help when needed, educating ourselves and others about mental health, and advocating for policy changes that prioritize accessible and affordable mental health services. Contact your representatives to support legislation that improves mental healthcare access. Let's work together to break down the barriers and ensure everyone has access to the mental health treatment they deserve.

Featured Posts
-
 Xrp Investment Weighing The Risks And Rewards Of Ripples Growth
May 02, 2025
Xrp Investment Weighing The Risks And Rewards Of Ripples Growth
May 02, 2025 -
 8000 Km A Velo Le Defi De Trois Jeunes Du Bocage Ornais
May 02, 2025
8000 Km A Velo Le Defi De Trois Jeunes Du Bocage Ornais
May 02, 2025 -
 Blay Styshn 6 Dlyl Shaml Llmelwmat Almtwfrt
May 02, 2025
Blay Styshn 6 Dlyl Shaml Llmelwmat Almtwfrt
May 02, 2025 -
 Pussy Riots Maria Alyokhina Brings Riot Day To Edinburgh Fringe
May 02, 2025
Pussy Riots Maria Alyokhina Brings Riot Day To Edinburgh Fringe
May 02, 2025 -
 Huntington Whiteleys White Lingerie Captivating Simplicity
May 02, 2025
Huntington Whiteleys White Lingerie Captivating Simplicity
May 02, 2025
Latest Posts
-
 Tory Chairman Condemns Farages Populism Yet Faces Reform Uk Challenges
May 03, 2025
Tory Chairman Condemns Farages Populism Yet Faces Reform Uk Challenges
May 03, 2025 -
 Rome Soupcons De Complot Macronien Pour L Election Papale
May 03, 2025
Rome Soupcons De Complot Macronien Pour L Election Papale
May 03, 2025 -
 L Intimite Macron Brigitte Des Confidences Apres Des Annees De Vie Commune
May 03, 2025
L Intimite Macron Brigitte Des Confidences Apres Des Annees De Vie Commune
May 03, 2025 -
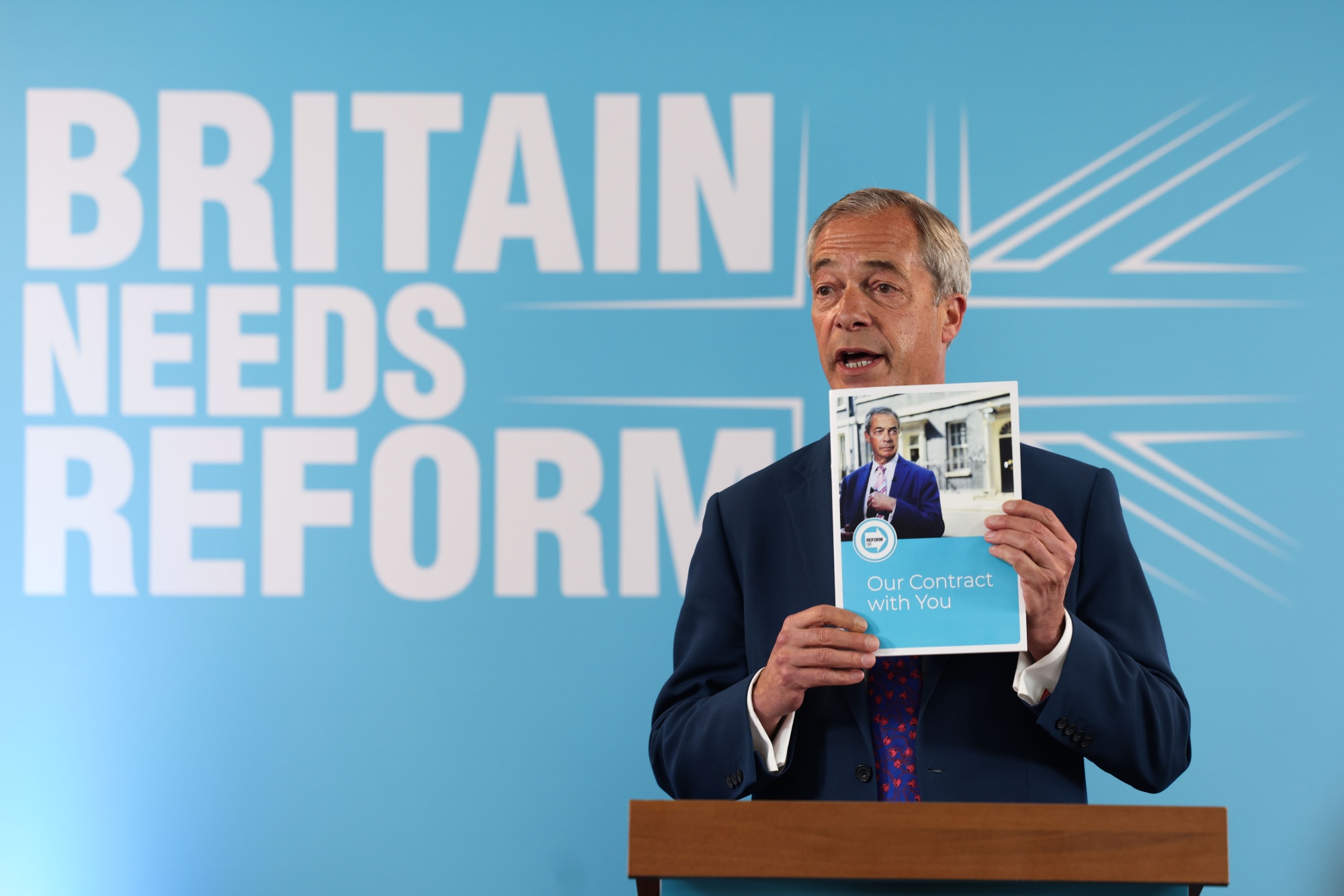 Reform Uk And The Conservatives The Chairmans Public Dispute On Populism
May 03, 2025
Reform Uk And The Conservatives The Chairmans Public Dispute On Populism
May 03, 2025 -
 Emmanuel Macron Et Brigitte Une Intimite Devoilee Apres Des Annees De Mariage
May 03, 2025
Emmanuel Macron Et Brigitte Une Intimite Devoilee Apres Des Annees De Mariage
May 03, 2025
