Metabolic Syndrome And Dementia: A Study Reveals The Impact Of Lifestyle Choices

Table of Contents
Understanding the Link Between Metabolic Syndrome and Dementia
Metabolic syndrome is a cluster of conditions—high blood pressure, high blood sugar, excess body fat around the waist, and abnormal cholesterol or triglyceride levels—that significantly increase the risk of heart disease, stroke, and type 2 diabetes. Emerging research strongly suggests a parallel increase in the risk of dementia. This connection isn't simply coincidental; several biological pathways explain the link.
H3: The Inflammatory Pathway
Chronic inflammation is a hallmark of MetS. This persistent inflammation damages brain cells and contributes to cognitive decline.
- Cytokines: These inflammatory proteins, elevated in individuals with MetS, can cross the blood-brain barrier, triggering neuroinflammation and damaging brain tissue.
- Oxidative Stress: MetS often leads to increased oxidative stress, an imbalance between free radicals and antioxidants, further exacerbating neuronal damage.
- Neuroinflammation: The sustained inflammatory response in the brain impairs synaptic function and neuronal survival, accelerating cognitive decline and increasing dementia risk. Studies like the one published in Neurobiology of Disease (2020) directly link elevated inflammatory markers in MetS patients to accelerated cognitive decline.
H3: Vascular Damage and Cognitive Impairment
MetS significantly contributes to vascular damage, compromising blood flow to the brain. This reduced cerebral perfusion is a critical factor in the development of dementia.
- Hypertension: High blood pressure damages blood vessels, leading to atherosclerosis and increasing the risk of stroke, a major cause of vascular dementia.
- Atherosclerosis: The buildup of plaque in arteries reduces blood flow to the brain, leading to ischemia and neuronal death. Research in the Lancet Neurology (2018) emphasizes the strong correlation between cerebrovascular disease and dementia risk in individuals with MetS.
H3: Insulin Resistance and Brain Function
Insulin resistance, a central feature of MetS, negatively impacts brain function.
- Insulin's Role in Brain Metabolism: Insulin plays a vital role in glucose transport across the blood-brain barrier, essential for neuronal function. Insulin resistance disrupts this process.
- Effects on Neuronal Plasticity and Memory: Impaired insulin signaling negatively affects synaptic plasticity and memory consolidation, contributing to cognitive decline. Studies published in Diabetes (2019) indicate a strong association between insulin resistance and an increased risk of Alzheimer's disease.
Lifestyle Modifications to Mitigate the Risk
Adopting a healthy lifestyle is crucial in mitigating the risk of both metabolic syndrome and dementia. Significant improvements can be achieved through targeted changes.
H3: Dietary Changes
A balanced diet plays a pivotal role.
- Mediterranean Diet: This diet, rich in fruits, vegetables, whole grains, and healthy fats, has shown significant benefits in improving metabolic health and reducing the risk of cognitive decline.
- Weight Management: Maintaining a healthy Body Mass Index (BMI) is crucial, as obesity is a significant risk factor for MetS.
H3: Regular Physical Activity
Regular exercise is beneficial for both physical and cognitive health.
- Aerobic Exercise: Activities like brisk walking, swimming, or cycling improve cardiovascular health and insulin sensitivity.
- Strength Training: Strength training improves muscle mass and bone density, further contributing to overall health.
- Flexibility Exercises: Yoga and stretching enhance flexibility, balance, and reduce stress. Regular exercise improves blood flow to the brain, reduces inflammation, and promotes neurogenesis (the formation of new brain cells).
H3: Stress Management Techniques
Chronic stress exacerbates metabolic dysfunction. Stress reduction techniques are essential.
- Mindfulness: Practicing mindfulness meditation helps regulate stress hormones and improve cognitive function.
- Yoga: Yoga combines physical postures, breathing techniques, and meditation to reduce stress and improve overall well-being.
- Effective stress management improves insulin sensitivity, reduces inflammation, and enhances cognitive performance.
Early Detection and Management of Metabolic Syndrome
Early detection and proactive management of MetS are crucial to reduce the risk of dementia.
H3: Regular Health Check-ups
Regular medical check-ups are vital for early detection.
- Blood Pressure: Regular blood pressure monitoring is essential.
- Blood Glucose: Regular blood glucose tests detect impaired glucose tolerance or diabetes.
- Cholesterol Levels: Monitoring cholesterol and triglyceride levels is crucial.
- Waist Circumference: Measuring waist circumference helps assess abdominal fat accumulation.
H3: Collaboration with Healthcare Professionals
A multidisciplinary approach is vital for effective management.
- Medication: Doctors may prescribe medication to manage high blood pressure, high cholesterol, or high blood sugar.
- Lifestyle Changes: Healthcare professionals can provide guidance and support for adopting healthy lifestyle changes.
- Monitoring: Regular monitoring of risk factors is crucial to assess the effectiveness of treatment and lifestyle modifications.
Conclusion
The strong link between metabolic syndrome and dementia is undeniable. Early detection and proactive lifestyle interventions are vital for reducing the risk. Key takeaways include the importance of a balanced diet, regular physical activity, and effective stress management. These modifications not only reduce the risk of MetS but also significantly protect your brain health. Take control of your metabolic health; reduce your risk of dementia. Learn more about the link between metabolic syndrome and dementia, and consult your doctor about strategies to improve your metabolic health and protect your cognitive well-being. Don't wait; proactive steps today can make a significant difference in your long-term health.

Featured Posts
-
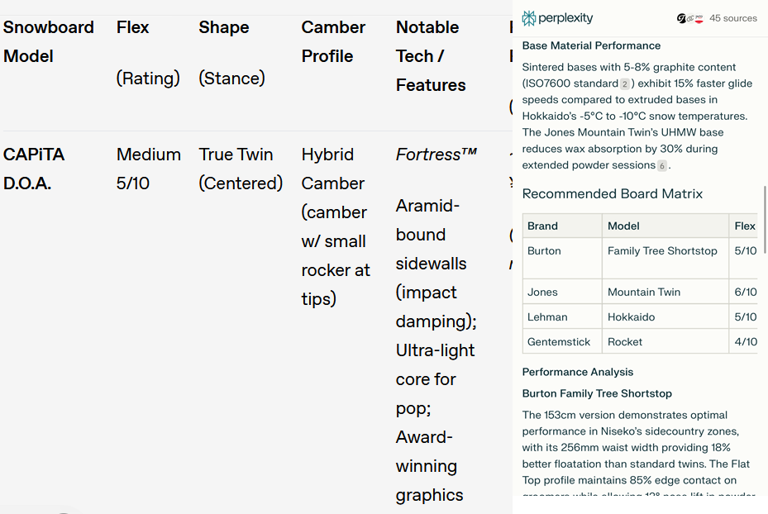 Perplexitys Potential Chrome Acquisition A Realistic Scenario If Google Divests
Apr 25, 2025
Perplexitys Potential Chrome Acquisition A Realistic Scenario If Google Divests
Apr 25, 2025 -
 Mateo Retegui Y La Competicion Por La Bota De Oro Un Analisis De Sus Goles
Apr 25, 2025
Mateo Retegui Y La Competicion Por La Bota De Oro Un Analisis De Sus Goles
Apr 25, 2025 -
 Top North East Destinations For Your Easter Break
Apr 25, 2025
Top North East Destinations For Your Easter Break
Apr 25, 2025 -
 Courtney Act And Tony Armstrong To Host Sbs Eurovision 2024
Apr 25, 2025
Courtney Act And Tony Armstrong To Host Sbs Eurovision 2024
Apr 25, 2025 -
 Mercer Internationals 2024 Financial Results And Dividend Declaration
Apr 25, 2025
Mercer Internationals 2024 Financial Results And Dividend Declaration
Apr 25, 2025
Latest Posts
-
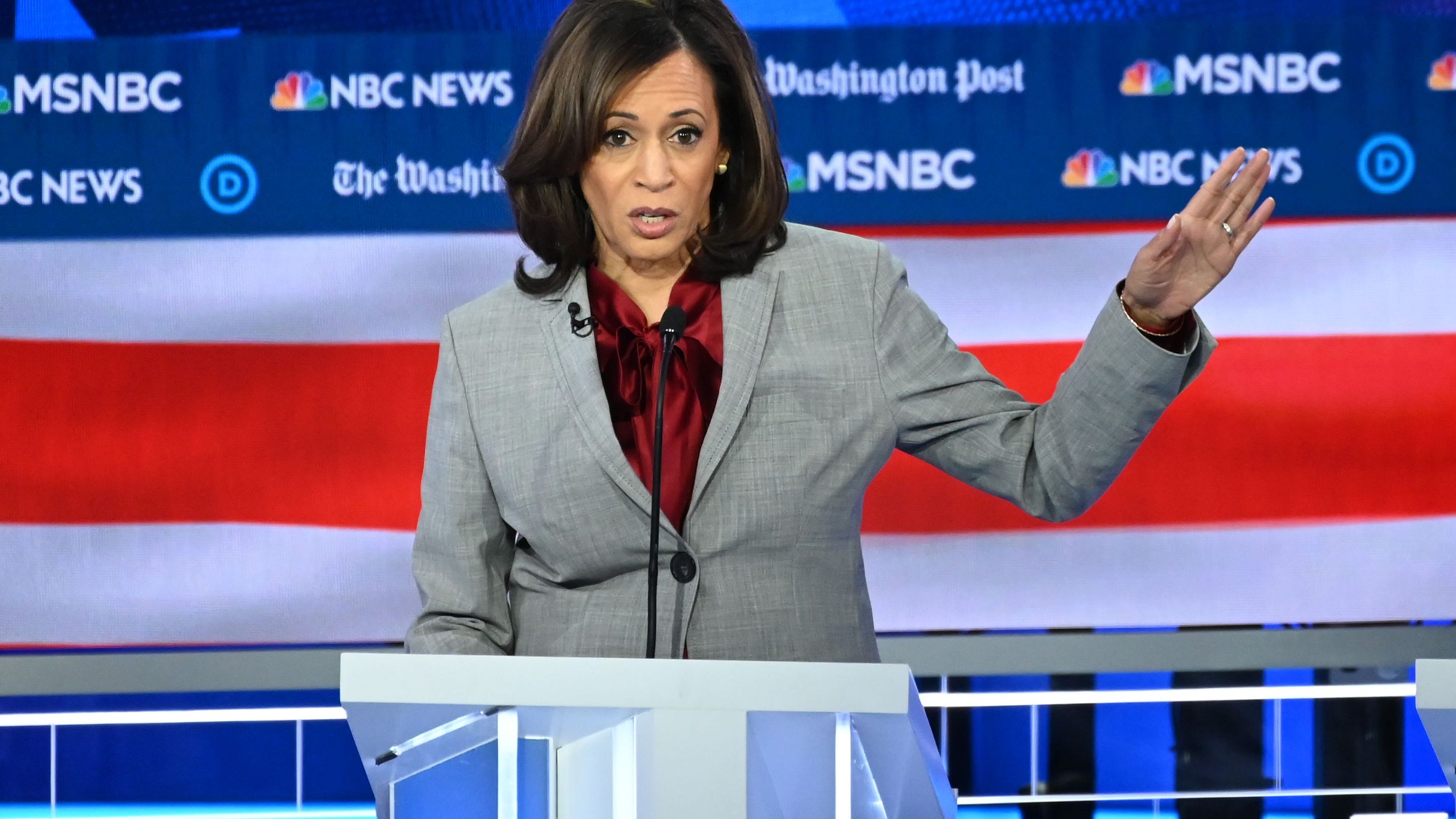 Democratic Insiders Criticize Kamala Harris Post Election Absence
Apr 30, 2025
Democratic Insiders Criticize Kamala Harris Post Election Absence
Apr 30, 2025 -
 Olivia Wilde 40 And Dane Di Liegro 36 Couples Pda At La Lakers Game
Apr 30, 2025
Olivia Wilde 40 And Dane Di Liegro 36 Couples Pda At La Lakers Game
Apr 30, 2025 -
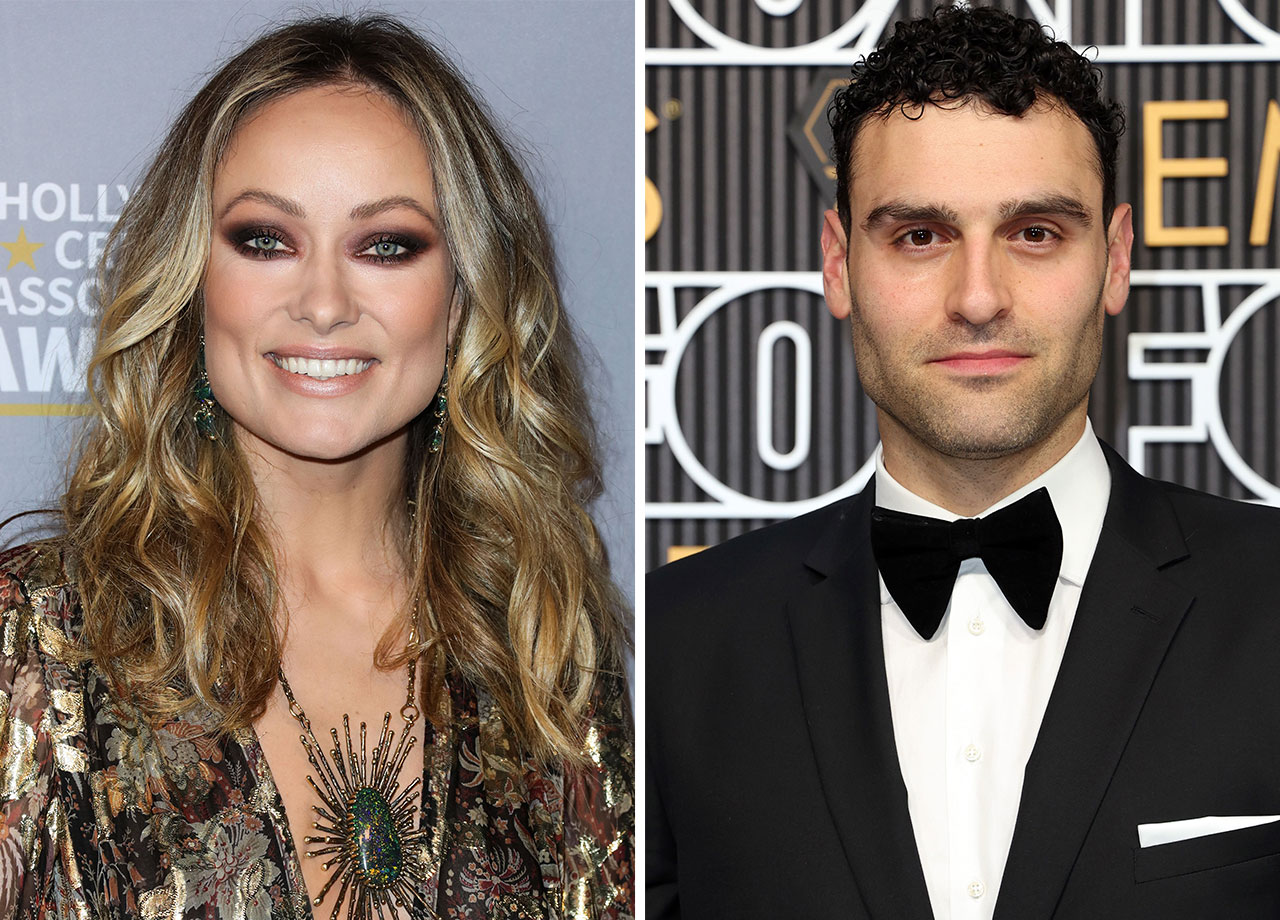 Olivia Wilde And Dane Di Liegros Relationship A Look At Their Recent Public Appearance
Apr 30, 2025
Olivia Wilde And Dane Di Liegros Relationship A Look At Their Recent Public Appearance
Apr 30, 2025 -
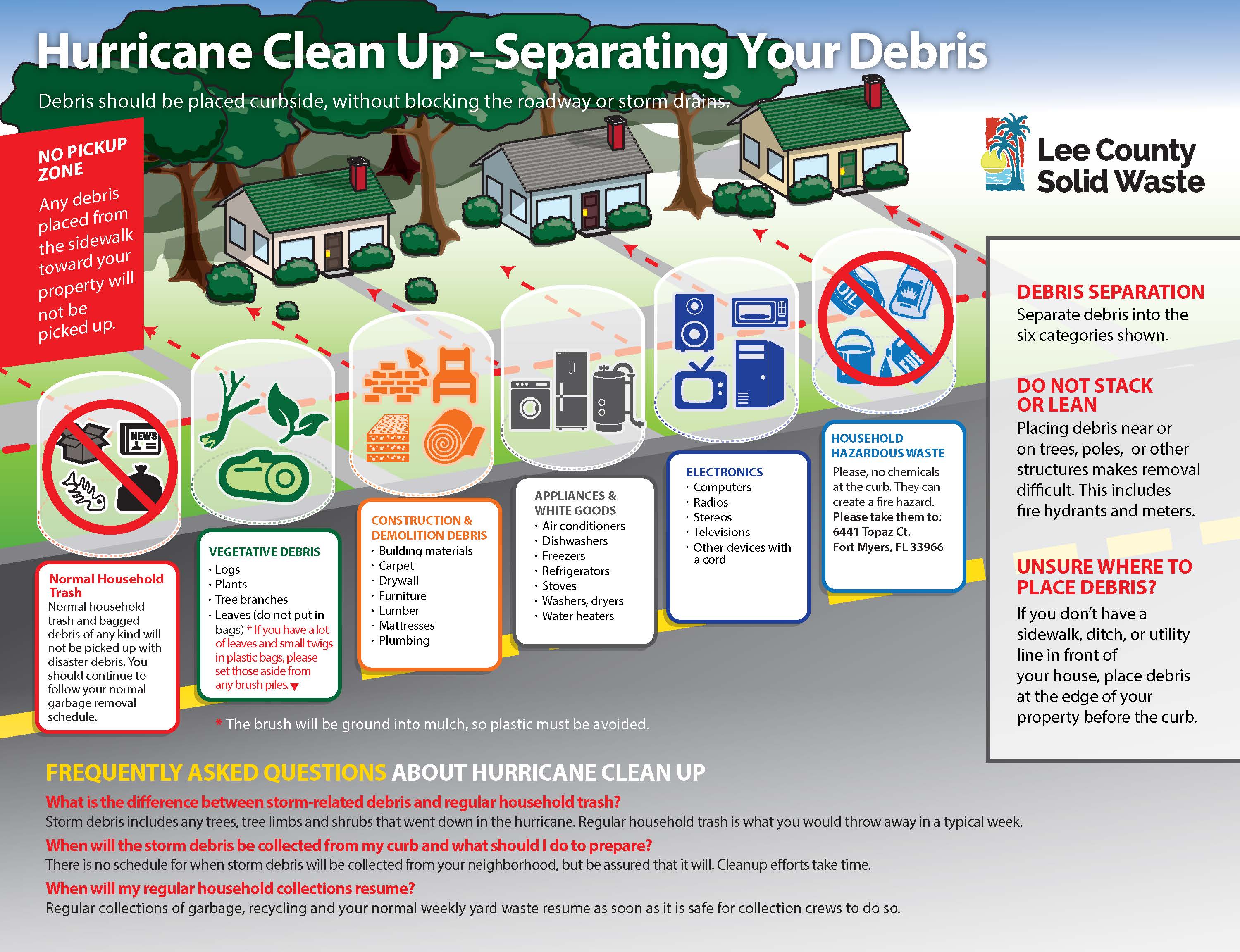 Louisville Launches Storm Debris Removal Program What You Need To Know
Apr 30, 2025
Louisville Launches Storm Debris Removal Program What You Need To Know
Apr 30, 2025 -
 Olivia Wilde And Dane Di Liegro Spotted Again Looking Loved Up At Lakers Game
Apr 30, 2025
Olivia Wilde And Dane Di Liegro Spotted Again Looking Loved Up At Lakers Game
Apr 30, 2025
