The State Of Mental Healthcare: Addressing Systemic Issues

Table of Contents
Lack of Access to Affordable and Quality Mental Healthcare
Many individuals face significant barriers to accessing affordable and quality mental healthcare. These barriers often intersect and exacerbate each other, creating a complex web of challenges for those seeking help.
Geographic Barriers
Geographic location plays a significant role in access to mental healthcare. Many individuals, particularly in rural or underserved communities, experience a critical lack of access to mental health professionals.
- Limited number of practitioners: The density of mental health professionals is often far lower in rural areas compared to urban centers.
- High travel costs and transportation limitations: Long distances, lack of reliable transportation, and the financial burden of travel significantly impede access to care. This is especially true for individuals with limited mobility or financial resources.
- Lack of telehealth infrastructure in remote areas: While telehealth offers a potential solution, reliable internet access and technological literacy remain barriers in many underserved areas. The digital divide directly impacts access to mental health services.
Financial Barriers
The high cost of mental healthcare creates significant barriers for many individuals and families. The financial burden can prevent individuals from seeking necessary treatment, leading to worsening symptoms and poorer health outcomes.
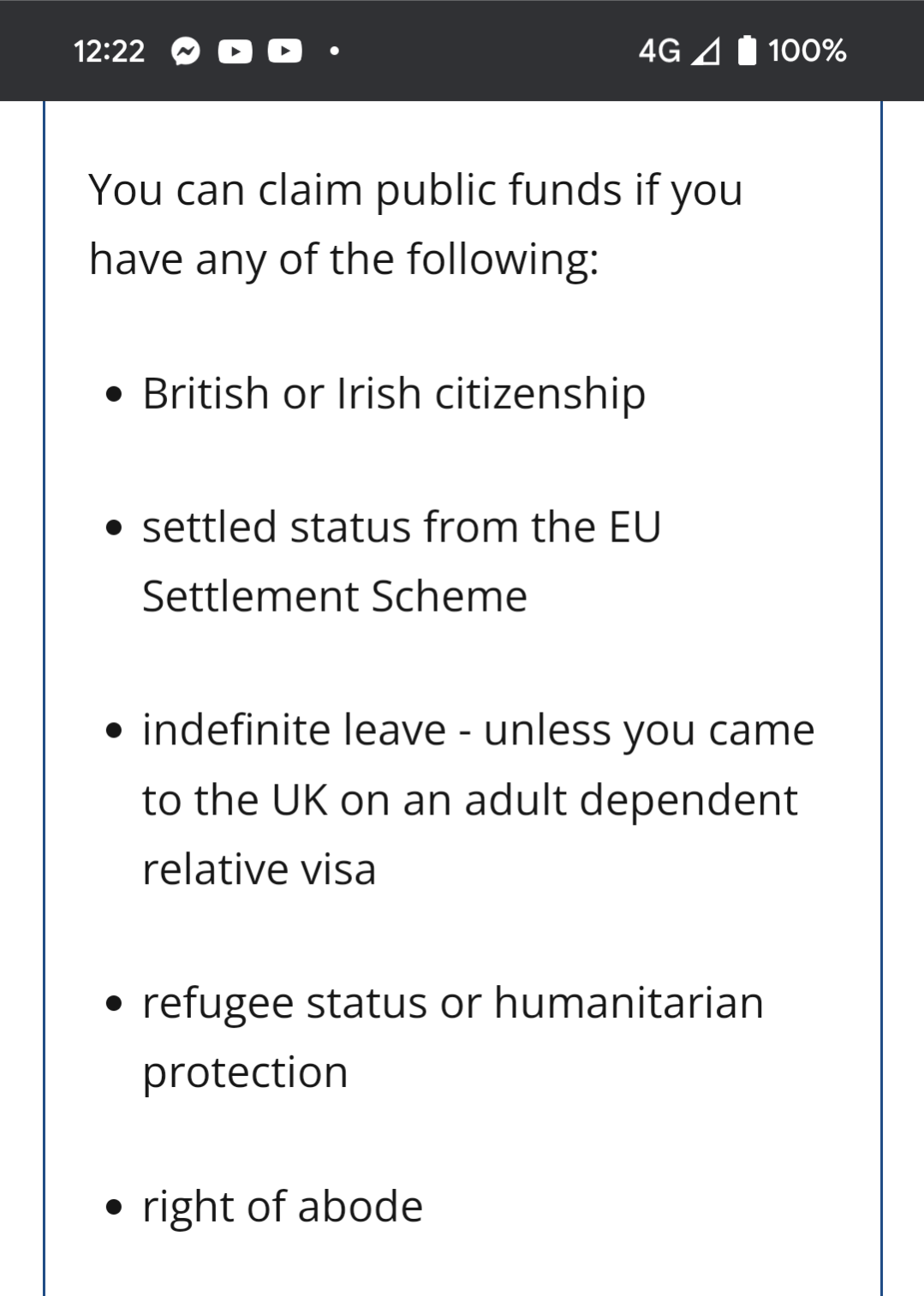
- Insufficient insurance coverage for mental health services: Many insurance plans offer inadequate coverage for mental health services, leading to high out-of-pocket expenses. This often results in individuals delaying or forgoing treatment altogether.
- High out-of-pocket expenses deterring treatment: Even with insurance, the cost of therapy, medication, and hospitalization can be prohibitive for many, especially those with low incomes.
- Limited availability of low-cost or free community mental health clinics: The scarcity of affordable or free clinics exacerbates the problem, leaving many vulnerable individuals without access to care.
Stigma and Discrimination
The pervasive stigma surrounding mental illness remains a major barrier to seeking help. This stigma manifests in various forms, preventing individuals from acknowledging their needs and accessing appropriate care.
- Fear of judgment from family, friends, and employers: The fear of social repercussions often prevents individuals from disclosing mental health concerns.
- Discriminatory practices in employment and housing: Stigma can lead to discrimination in the workplace and housing, further isolating and marginalizing individuals with mental health conditions.
- Lack of public awareness and education surrounding mental health: A lack of understanding and empathy contributes to the perpetuation of stigma. Increased public awareness and education are crucial to combatting this issue.
Shortage of Mental Health Professionals
A critical shortage of mental health professionals, coupled with high burnout rates, further exacerbates access issues. This shortage disproportionately impacts underserved communities.
Burnout and Turnover
The demanding nature of mental health work, combined with inadequate resources and support, leads to high rates of burnout and turnover among professionals.
- Inadequate compensation and benefits: Low salaries and limited benefits make it challenging to attract and retain qualified mental health professionals.
- Limited access to support and supervision for practitioners: The lack of adequate support and supervision contributes to burnout and can negatively impact the quality of care provided.
- Significant administrative burden reducing time spent with patients: Excessive paperwork and administrative tasks reduce the time practitioners can dedicate to providing direct patient care.
Unequal Distribution of Professionals
Mental health professionals tend to concentrate in urban areas, leaving rural and underserved communities with severely limited access.
- Need for increased recruitment and training programs in underserved areas: Targeted recruitment and training initiatives are essential to address the disparities in professional distribution.
- Incentivizing professionals to work in rural and underserved communities: Offering financial incentives, loan forgiveness programs, and other benefits can encourage professionals to work in underserved areas.
- Expansion of telehealth services to improve access: Telehealth can help bridge geographical barriers and improve access to mental healthcare in remote areas.
Inadequate Integration of Mental Healthcare into Primary Care
Integrating mental healthcare into primary care settings is essential for early intervention and comprehensive care, yet significant challenges remain.
Lack of Collaboration
Limited collaboration between primary care physicians (PCPs) and mental health professionals hinders early detection and effective management of mental health conditions.
- Need for improved communication and referral pathways: Streamlined referral processes and clear communication between PCPs and mental health specialists are crucial.
- Integration of mental health screenings into primary care settings: Routine mental health screenings in primary care can help identify individuals who may benefit from early intervention.
- Training primary care physicians to identify and manage common mental health concerns: Equipping PCPs with the skills to identify and manage common mental health issues can improve early intervention and reduce the burden on specialized mental health services.
Insufficient Resources
Primary care settings often lack the resources and expertise necessary to provide adequate mental healthcare.
- Need for increased funding for mental health services within primary care: Increased funding can support the integration of mental health professionals into primary care teams.
- Support for collaborative care models integrating mental health professionals into primary care teams: Collaborative care models, where mental health professionals work alongside PCPs, can improve the quality and efficiency of care.
- Development of effective, brief interventions for primary care settings: Developing and implementing brief interventions in primary care settings can address common mental health concerns efficiently.
Policy and Systemic Reforms Needed for Improved Mental Healthcare
Comprehensive policy and systemic reforms are essential to address the systemic issues impacting mental healthcare.
Increased Funding for Mental Health Research and Services
Significant investment in research and services is crucial to expand access and improve the quality of mental health care. This funding should support a wide range of initiatives, including workforce development, service expansion, and research into new treatments and prevention strategies.
Strengthening Mental Health Parity Laws
Enforcing existing mental health parity laws to ensure equal coverage for mental and physical health is critical. This requires robust oversight and enforcement mechanisms to prevent discriminatory practices by insurance providers.
Expanding Access to Telehealth
Utilizing telehealth technology can overcome geographical barriers and improve access to care for individuals in underserved areas. This requires investment in infrastructure and training to ensure equitable access for all.
Addressing Stigma through Public Awareness Campaigns
Reducing stigma through public awareness campaigns and education programs is vital to encourage individuals to seek help and support. These campaigns must be inclusive and address the specific needs of diverse communities.
Conclusion
The state of mental healthcare is undeniably a crisis. Addressing the systemic issues outlined above requires a multifaceted approach encompassing increased funding, policy reforms, improved access to professionals, and a concerted effort to reduce stigma surrounding mental illness. We must prioritize comprehensive mental healthcare reform to ensure equitable access to quality care for all. Let’s work together to improve the mental healthcare system and create a future where everyone has the support they need to thrive. We must demand better mental health services and advocate for change in our communities. Join the movement to improve mental health access for all.

Featured Posts
-
 2024s Underrated Game Lands On Ps Plus This Month
May 02, 2025
2024s Underrated Game Lands On Ps Plus This Month
May 02, 2025 -
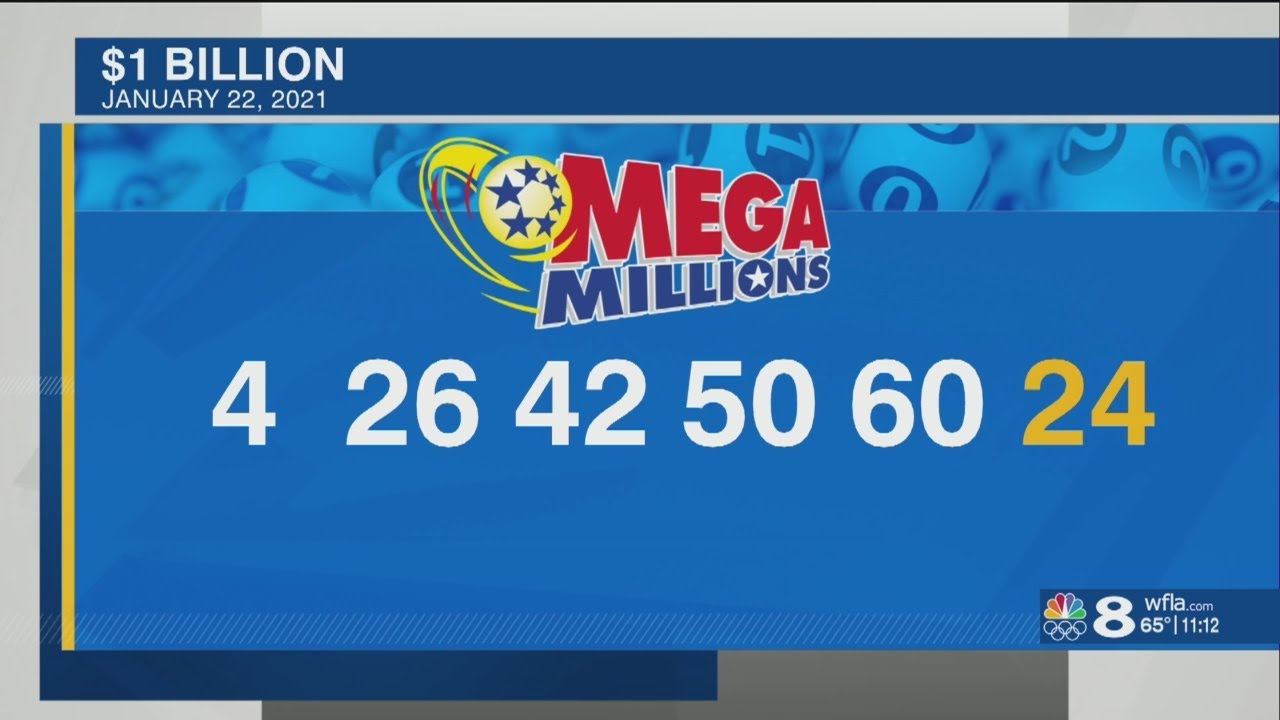 Daily Lotto Friday April 18th 2025 Winning Numbers
May 02, 2025
Daily Lotto Friday April 18th 2025 Winning Numbers
May 02, 2025 -
 Time Is Running Out Get Your Free Fortnite Cowboy Bebop Items
May 02, 2025
Time Is Running Out Get Your Free Fortnite Cowboy Bebop Items
May 02, 2025 -
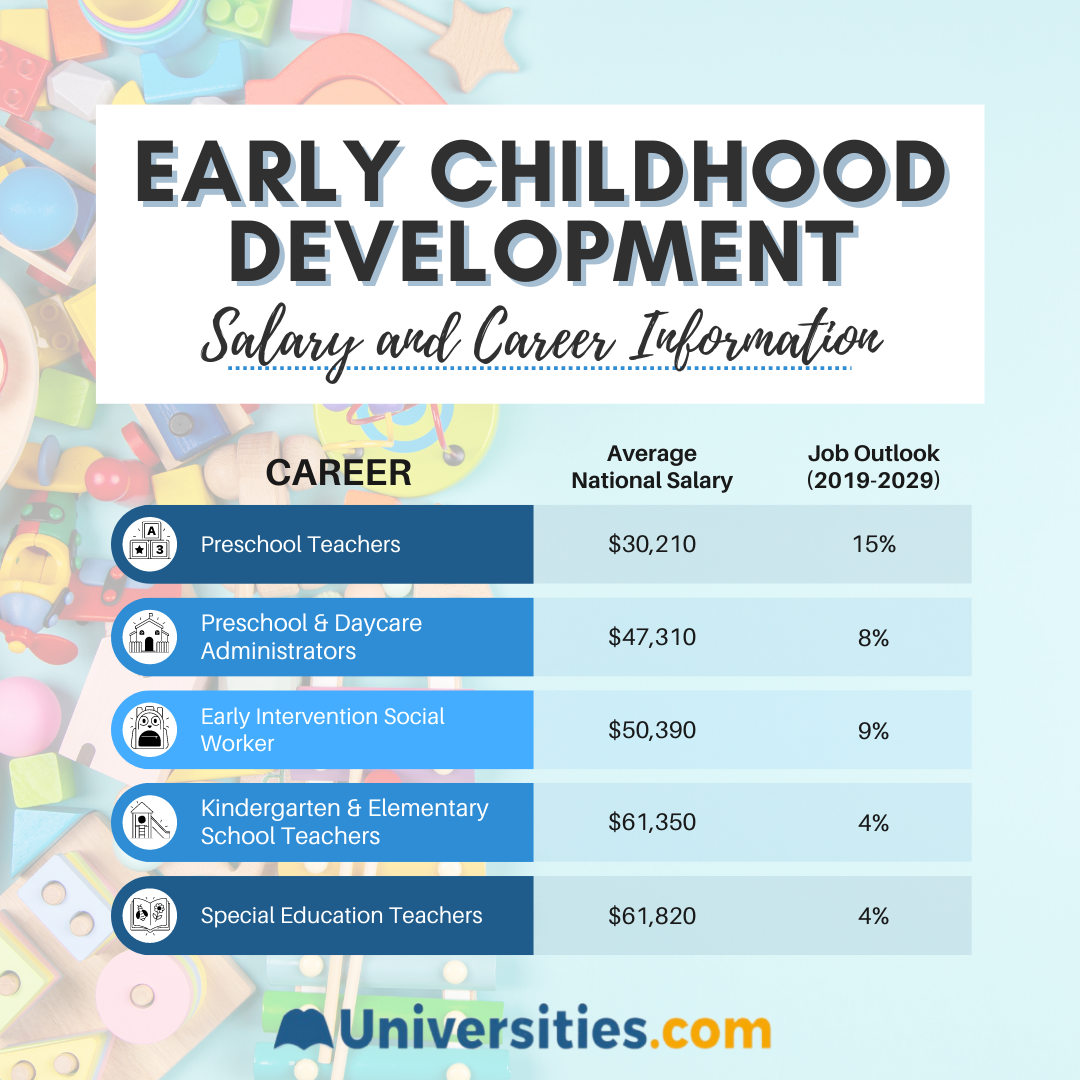 Investing In Early Childhood Development A Foundation For Strong Mental Health
May 02, 2025
Investing In Early Childhood Development A Foundation For Strong Mental Health
May 02, 2025 -
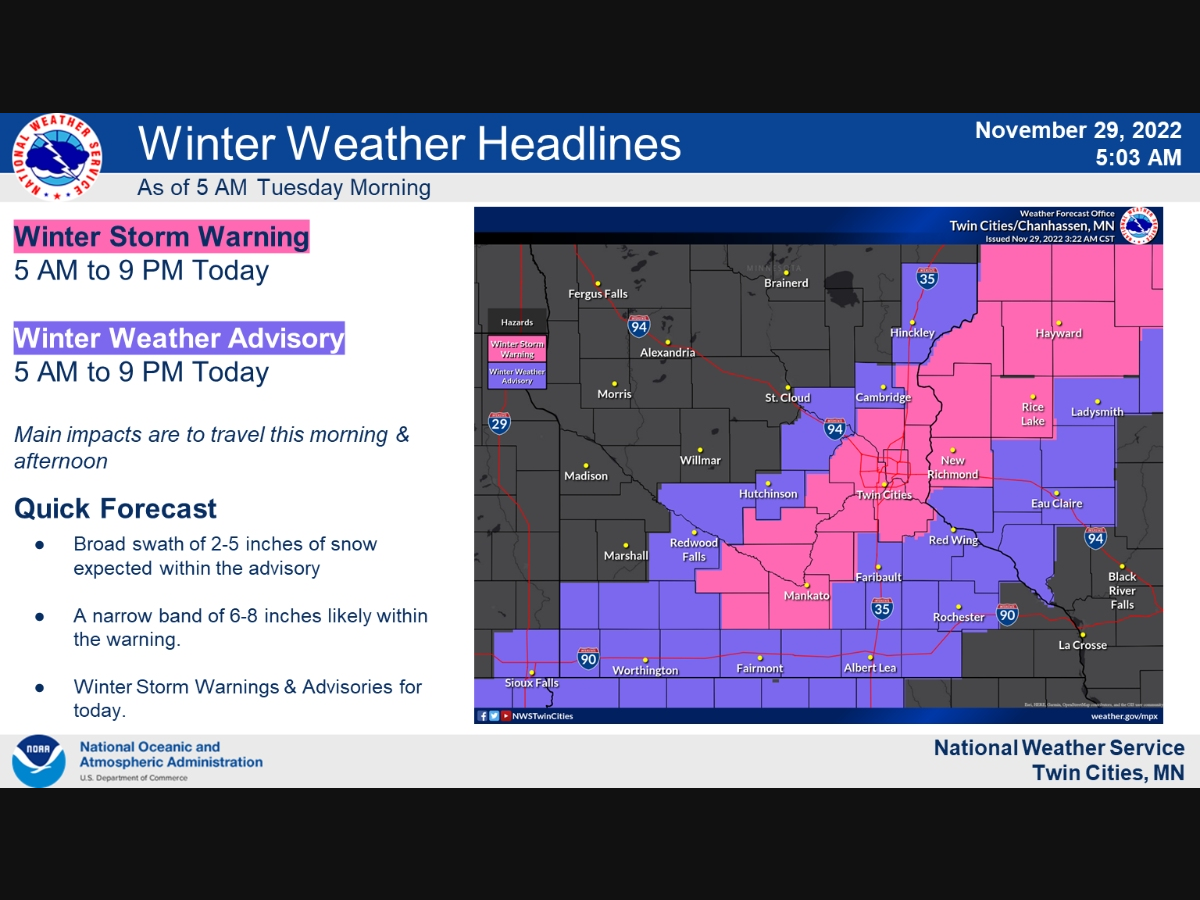 Severe Winter Weather Alert Four Inches Of Snow And Bitter Cold On Tuesday
May 02, 2025
Severe Winter Weather Alert Four Inches Of Snow And Bitter Cold On Tuesday
May 02, 2025
Latest Posts
-
 Labours Image Problem A Deep Dive Into The Nasty Party Accusation
May 03, 2025
Labours Image Problem A Deep Dive Into The Nasty Party Accusation
May 03, 2025 -
 Assessing Reform Uks Credibility On Agricultural Issues
May 03, 2025
Assessing Reform Uks Credibility On Agricultural Issues
May 03, 2025 -
 Analysis Guido Fawkes Take On Revised Energy Policies
May 03, 2025
Analysis Guido Fawkes Take On Revised Energy Policies
May 03, 2025 -
 Is Labour Becoming The Nasty Party A Political Analysis
May 03, 2025
Is Labour Becoming The Nasty Party A Political Analysis
May 03, 2025 -
 Will Reform Uks Policies Benefit Uk Farming An In Depth Look
May 03, 2025
Will Reform Uks Policies Benefit Uk Farming An In Depth Look
May 03, 2025
