Uterine Transplantation: A Children's Hospital Activist's Perspective On Transgender Pregnancy
Table of Contents
The Current State of Uterine Transplantation
Uterine transplantation, also known as uterus transplantation, is a relatively new and complex surgical procedure. While offering hope to individuals unable to carry a pregnancy, its success rates remain limited. The procedure involves transplanting a healthy uterus from a donor into a recipient, enabling the recipient to potentially conceive and carry a child to term.
- Success rates and limitations: While successful live births have been achieved following uterine transplantation, success rates are still relatively low compared to other transplant procedures. Many factors influence success, including the health of the donor and recipient, the surgical technique, and post-operative care. Rejection of the transplanted uterus remains a significant challenge.
- Ethical considerations around donor selection and recipient eligibility: The ethical considerations surrounding uterine transplantation are significant. Careful selection of both donors and recipients is crucial, ensuring informed consent and minimizing risks. Criteria for eligibility often include factors such as age, overall health, and psychological well-being.
- Long-term health implications for both donor and recipient: Both the donor and recipient face potential long-term health implications. Donors undergo major surgery with associated risks, while recipients face the possibility of rejection, infection, and other complications. Long-term follow-up is crucial for both.
- Cost and accessibility of uterine transplantation: The high cost of uterine transplantation, including surgery, hospitalization, immunosuppression medications, and ongoing monitoring, significantly limits accessibility. Insurance coverage varies widely, creating significant financial barriers for many potential recipients.
Transgender Pregnancy and Access to Reproductive Technologies
Transgender women seeking pregnancy face numerous challenges in accessing reproductive technologies. While IVF (in-vitro fertilization) and surrogacy are options, they are often expensive, inaccessible, and fraught with legal and social barriers. Uterine transplantation offers a potential, albeit still experimental, alternative pathway to pregnancy for transgender women.
- Legal and societal barriers to access: Legal frameworks regarding reproductive rights for transgender individuals vary widely across jurisdictions. Some countries or states may not recognize transgender women's legal right to access reproductive technologies, creating significant obstacles. Societal stigma and discrimination can also add layers of complexity.
- Financial constraints and insurance coverage: The high cost of IVF, surrogacy, and potentially uterine transplantation creates significant financial barriers. Insurance coverage for these procedures is often inconsistent and limited, making access difficult for many transgender women.
- Psychological and emotional toll of navigating the system: The process of navigating the healthcare system, facing legal hurdles, and managing the emotional complexities of infertility can be incredibly stressful and emotionally draining for transgender women.
- The role of advocacy groups and activists in improving access: Advocacy groups and activists play a vital role in raising awareness, challenging discriminatory practices, and advocating for policy changes that improve access to reproductive healthcare for transgender individuals.
The Role of Children's Hospitals in Advocacy
Children's hospitals, with their focus on family-centered care, are uniquely positioned to advocate for transgender individuals' access to reproductive healthcare. Their commitment to family well-being extends beyond biological definitions of family, recognizing the importance of creating inclusive and supportive environments for all.
- Children's hospitals' focus on family-centered care: The core values of family-centered care emphasize inclusivity and respect for diverse family structures. This philosophy naturally extends to supporting transgender individuals seeking to build families.
- The importance of inclusive policies and practices: Implementing inclusive policies and providing culturally competent care are essential for creating a welcoming and supportive environment for transgender patients and their families within children's hospitals.
- The potential for children's hospitals to lead in research and education: Children's hospitals can take a leadership role in funding research into reproductive technologies for transgender individuals and in educating healthcare professionals about transgender health issues.
- Collaborations between children's hospitals and LGBTQ+ organizations: Collaboration with LGBTQ+ organizations is vital for developing culturally sensitive programs, providing support services, and ensuring that care is aligned with the needs and experiences of transgender patients.
Ethical Considerations and Future Directions
Uterine transplantation for transgender individuals raises complex ethical questions that require careful consideration. These ethical considerations are vital for responsible development and implementation of this emerging technology.
- Informed consent and patient autonomy: Ensuring fully informed consent is paramount, ensuring that potential recipients understand the risks, benefits, and limitations of the procedure, allowing for autonomous decision-making.
- Potential long-term effects on the child and family: The potential long-term psychological and physical effects on the child born through uterine transplantation need to be thoroughly researched and addressed.
- Societal implications and potential for discrimination: The societal impact of uterine transplantation for transgender individuals needs careful consideration, addressing potential for discrimination and ensuring social support for families formed through this technology.
- The need for ongoing research and ethical guidelines: Continued research is crucial to refine surgical techniques, improve success rates, and address the long-term consequences for all involved. Clear ethical guidelines are necessary to guide practice and ensure equitable access.
Conclusion
Understanding the ethical considerations and challenges surrounding uterine transplantation and transgender pregnancy is vital. The current state of uterine transplantation technology presents both opportunities and limitations for transgender women seeking pregnancy. Access to reproductive technologies, including IVF, surrogacy, and potentially uterine transplantation, remains significantly limited by financial, legal, and societal barriers. Children's hospitals, with their commitment to family-centered care, have a crucial role to play in advocating for inclusive healthcare policies and practices that support all individuals in their pursuit of parenthood. Let's advocate for inclusive healthcare policies that support all individuals in their pursuit of parenthood, ensuring equitable access to advancements in uterine transplantation and other transgender pregnancy options.
Featured Posts
-
 Fusion Renaissance Modem Elisabeth Borne Clarifie La Ligne Gouvernementale
May 10, 2025
Fusion Renaissance Modem Elisabeth Borne Clarifie La Ligne Gouvernementale
May 10, 2025 -
 David Gentile Gpb Capital Founder Receives 7 Year Sentence For Fraud
May 10, 2025
David Gentile Gpb Capital Founder Receives 7 Year Sentence For Fraud
May 10, 2025 -
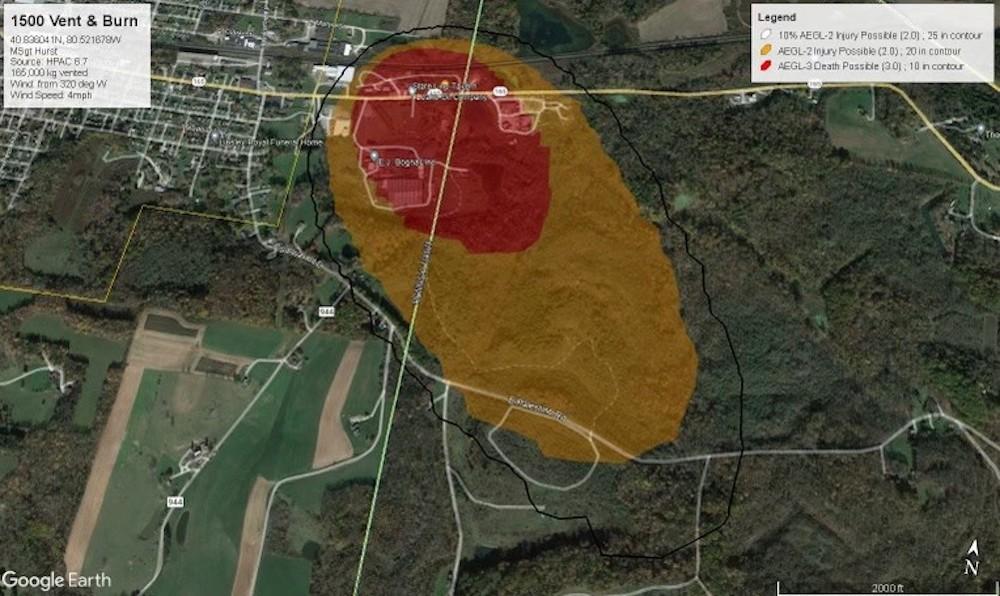 Ohio Train Derailment The Long Term Impact Of Toxic Chemical Exposure
May 10, 2025
Ohio Train Derailment The Long Term Impact Of Toxic Chemical Exposure
May 10, 2025 -
 Palantir Stock Before May 5th Is Wall Streets Prediction Accurate
May 10, 2025
Palantir Stock Before May 5th Is Wall Streets Prediction Accurate
May 10, 2025 -
 From Wolves To The Summit A Footballers Inspiring Success Story
May 10, 2025
From Wolves To The Summit A Footballers Inspiring Success Story
May 10, 2025
